| Download this report in PDF format |
The members of the Management and Therapy Subcommittee undertook an evidence-based review of current dry eye therapies and management options. Management options reviewed in detail included treatments for tear insufficiency and lid abnormalities, as well as anti-inflammatory medications, surgical approaches, dietary modifications, environmental considerations and complementary therapies. Following this extensive review it became clear that many of the treatments available for the management of dry eye disease lack the necessary Level 1 evidence to support their recommendation, often due to a lack of appropriate masking, randomization or controls and in some cases due to issues with selection bias or inadequate sample size.
Reflecting on all available evidence, a staged management algorithm was derived that presents a step-wise approach to implementing the various management and therapeutic options according to disease severity. While this exercise indicated that differentiating between aqueous-deficient and evaporative dry eye disease was critical in selecting the most appropriate management strategy, it also highlighted challenges, based on the limited evidence currently available, in predicting relative benefits of specific management options, in managing the two dry eye disease subtypes.
Further evidence is required to support the introduction, and continued use, of many of the treatment options currently available to manage dry eye disease, as well as to inform appropriate treatment starting points and understand treatment specificity in relation to dry eye disease subtype.
Keywords: Dry eye disease; Dry eye workshop; Management; TFOS DEWS II; Therapy
Historically, DED was considered to be largely due to tear insufficiency and was treated by prescribing tear replacement products or by conserving the tears via punctal plugs. More recent treatments have included the use of methods to stimulate tears.
Tear replacement with ocular lubricants is traditionally considered a mainstay of DED therapy and there are numerous topical formulations available. Over-the-counter (OTC) products are often termed “artificial tears” which, as their name suggests, attempt to replace and/or supplement the natural tear film. However, these products do not target the underlying pathophysiology of DED, and the mechanisms of any palliative actions are generally poorly understood.
Tear substitutes comprise a wide variety of products, which typically aim to target one or more layers of the tear film. The wide variety of properties of these ocular lubricants has been reviewed elsewhere [11–15].
Ocular lubricants are largely regarded as safe, although there are some reported side effects, most notably blurred vision, variable levels of “ocular discomfort” and foreign body sensation [16]. There are relatively few randomized controlled trials (RCTs) that have compared the relative superiority of a particular OTC product to others for DED therapy [17]. A recent Cochrane systematic review, which sought to evaluate the effect of OTC tear supplement products for treating DED, included 43 randomized controlled trials that had compared artificial tear formulations to no treatment, or placebo [16]. The primary outcome measure was patient-reported symptoms. The authors reported that the overall quality of evidence was low for the various tear supplement formulations compared in the review, and concluded that while artificial tears may be effective for treating DED, there was still a need for future research to enable robust conclusions to be drawn about the effectiveness of individual OTC artificial tear formulations.
While ocular lubricant formulations may vary in osmolarity, viscosity and pH, most share similarities in their major components. The most abundant component in lubricant eye drops is the aqueous base. To enhance lubrication and prolong the retention time on the ocular surface, a variety of viscosity enhancing agents are frequently incorporated.
The viscosity-enhancing agents used in tear supplement formulations include carbomer 940 (polyacrylic acid), carboxymethyl cellulose (CMC), dextran, hyaluronic acid (HA), HP-guar, hydroxypropyl methylcellulose (HPMC), polyvinyl alcohol (PVA), polyvinylpyrrolidone (PVP) and polyethylene glycol.
Viscosity enhancers are considered beneficial to the ocular surface in DED through a range of reported mechanisms. These include increasing tear film thickness, protecting against desiccation, promoting tear retention at the ocular surface, protecting the ocular surface, maintaining physiological corneal thickness, improving goblet cell density and relieving dry eye symptoms [18,19]. Although there are scores of formulations and products available, which vary by geographic region, there does not appear to be any substantial difference in effectiveness among them [16,20]. However, the differences in the viscosity of the drops can influence utilization. Eye drops with high viscosity can increase retention time on the ocular surface, but may also cause transient visual disturbances and result in unwanted debris on the eyelids and lashes, leading to decreased tolerance and compliance. Very high viscosity eye drops are typically recommended for overnight use, with low-viscosity drops being used in the daytime.
CMC is a cellulose derivative with carboxymethyl groups and is formed from the cell walls of plants. It is often used as its sodium salt, sodium carboxymethyl cellulose, and is also termed carmellose sodium. It is a very commonly used viscosity-enhancing agent in ocular lubricants as well as in pharmaceuticals, foods and cosmetics [21].
CMC can bind to corneal epithelial cells and promote epithelial cell healing [22,23]. CMC-based products have been proven to be successful in the management of mild-to-moderate dry eye in a number of studies [24–26].
Cellulose ethers are viscoelastic polysaccharides that increase the viscosity of the tears. Of these, HPMC has been used for many years in artificial lubricants and remains one of the most common ingredients. It is available in a wide variety of concentrations (from 0.2 to 0.8%) and is used in combination with many other components in modern ocular lubricants [11,14]. Due to its wide availability and use over many years, multiple studies have explored its potential to manage patients with DED [16]. A review of its performance shows that it is a safe and effective lubricant for those with low-to-moderate symptoms of DED [16].
Hyaluronic acid (HA), also termed hyaluron and sodium hyaluronate, is a naturally occurring anionic, non-sulfated glycosaminoglycan that is distributed widely throughout connective, epithelial, and neural tissues. It can be very large, with its molecular weight often reaching several million Daltons. HA is an important component of articular cartilage and is found in abundance in synovial fluid around joints, in the vitreous and aqueous humour [27]. A number of studies have demonstrated its ability to bind to ocular surface cells and its potential wound healing properties [28–33].
HA is used in a variety of tear supplements to increase viscosity and provide enhanced lubrication. HA exhibits non-Newtonian shear-thinning properties [34], where viscosity varies with shear rate. For HA-based solutions, the viscosity decreases with increasing shear rate, as occurs during a blink.
As the range of commercial products that contain HA increases, a growing number of Level 1 and 2 clinical studies have been published that demonstrate good tolerability and the ability to improve dry eye symptoms [35–42].
As described above, there are a number of publications supporting the use of topical drops that contain CMC or HA in the management of DED. Optive Fusion™ (Allergan, Parkway Parsippany, NJ, USA)) contains a combination of 0.5% CMC and 0.1% HA in a single topical formulation. In a murine dry eye study, mice administered CMC + HA topically showed significantly lower corneal fluorescein staining and higher goblet cell density than mice treated with drops containing CMC or HA alone [43]. In a 3-month, double-masked, multicenter study involving 305 subjects with DED, the commercially available combination of CMC + HA improved symptoms and signs of DED more than a commercially available topical formulation based on CMC alone [44].
HP-guar is a non-ionic, polymeric thickener that can rapidly confer high viscosity, through a pH-dependent process [45,46]. One HP-guar-based product, Systane® ULTRA (Alcon, Ft Worth, TX, USA), includes two demulcents (polyethylene glycol 400 and propylene glycol), and sorbitol, and is buffered with borate, resulting in a partially crosslinked borate/HP-guar gel in the bottle [47]. The pH of Systane ULTRA is 7.9 but when instilled onto the ocular surface, the reduction in pH, and dilution of the sorbitol concentration, increases the density of the borate/hydroxypropyl-guar crosslinks, producing a very low viscosity gel [45].
HP-guar-based products have been shown to improve dry eye symptoms, increase mucous layer thickness, reduce inflammation and protect the ocular surface [47–53].
A formulation containing the demulcents propylene glycol and polyethylene glycol and a dual polymer combination of HA and HP-guar (Systane® ULTRA HYDRATION; Alcon, Ft Worth, TX, USA) has been shown to be effective in desiccation protection and retention on the ocular surface in a corneal cell-based laboratory study [54].
The concept of using a dissolvable hydroxypropyl cellulose insert on the ocular surface to manage DED was first approved by the Food and Drug Administration (FDA) over 30 years ago, but for many years lost favour due to discomfort and relatively poor efficacy [55]. The newest version of this concept is LACRISERT™ (Bausch & Lomb, Rochester, NY, USA), which is a sterile, translucent, rod-shaped, water soluble, preservative-free, slow-release lubricant that is placed into the inferior cul-de-sac with the aid of a reusable applicator. It begins to soften within minutes, dissolving over the course of about 12 h and thickening the precorneal tear film. It is recommended for use in patients with moderate to severe DED, is usually inserted once a day and is contraindicated in patients who are hypersensitive to hydroxypropyl cellulose.
A multicenter, 2-visit, open-label, 4-week study was conducted to determine the acceptability of the inserts in 520 subjects with DED [56]. There was a significant improvement in symptoms, corneal fluorescein staining, conjunctival staining and tear volume. Contact lens wearers reported significant improvements, similar to non-wearers. Reported complications include transient blurring of vision, discomfort or irritation (particularly if not located appropriately), expulsion in patients with shallow conjunctival fornices and matting or stickiness of the eyelashes.
The original TFOS DEWS report drew attention to the importance of tear osmolarity, demonstrating that raised tear osmolarity is associated with DED [57]. Since that time, many studies have examined the link between DED and osmolarity. However, relatively few studies have investigated the impact of tear supplement hypo- or hyper-osmolar drops on tear osmolarity and any improvements in DED. Gilbard conducted a number of experiments to show that the use of a hypo-osmolar ocular lubricant could reverse various ocular surface changes (notably reduced goblet cell density) induced in a dry eye rabbit model [58–60]. Two more recent studies using hypotonic hyaluronic acid-based ocular lubricants demonstrated an improvement in both symptoms and various signs of DED [61,62]. However, more studies linking the ability of lubricants to reduce tear film osmolarity and their impact upon DED symptoms and signs are warranted.
A number of published studies demonstrate the potential to improve tear osmolarity with DED treatments [63–70], even in the absence of a change [71,72], or in association with negative outcomes [68,73,74], in other clinical features.
Since the publication of the first TFOS DEWS report, several examples of tracking dry eye therapy with tear osmolarity have been published. A study investigating the effects of a combination therapy of methylprednisolone and preservative-free 0.1% HA four times a day demonstrated a significant reduction in osmolarity at eight weeks that paralleled significant reductions in IL-1β and IL-8, as well as tear break up time (TBUT), corneal and conjunctival staining [75]. The authors concluded that measuring the changes in cytokine levels and tear osmolarity could objectively evaluate the anti-inflammatory effects of topical methylprednisolone applied in the treatment of patients with moderate to severe dry eye syndrome. A similar eight-week trial of a modified HA applied three times daily resulted in significant improvements in Ocular Surface Disease Index (OSDI) score, TBUT, conjunctival goblet cell density, corneal and conjunctival damage and tear osmolarity [66].
Tear osmolarity has also been shown to parallel improvements in dry eye symptoms and signs when patients use topical cyclosporine [63,76,77], HA [40,66,78–80], osmoprotective drops [40,67,69], and PEG/HP-Guar drops [81].
Osmoprotectants (e.g., L-carnitine and betaine) are a group of compatible solutes that protect cells under extreme osmotic stress by balancing the osmotic pressure without disturbing cell metabolism [82–85]. The osmoprotective effect depends on the amount of drug uptake and its retention time, and combinations of osmoprotectants with different pharmaceutical kinetics may function better than individual osmoprotectants.
There are a number of studies demonstrating that osmoprotectants have a beneficial effect on the treatment of DED. An in vitro study showed that the osmoprotectants L-carnitine and erythritol can protect cultured human corneal epithelial cells from hyperosmolar conditions by lowering levels of activated mitogen-activated protein kinases [86]. The osmoprotectants also showed inflammatory-suppressing properties under hyperosmotic stress [87]. A dry eye mouse study showed that osmoprotectants can reduce corneal staining, decrease cell apoptosis and inflammatory cytokines and increase the number of goblet cells [88].
Trehalose is a naturally occurring dissacharide, present in numerous non-mammalian species, which allows cells to survive in unfavorable environments. It is implicated in anhydrobiosis, which relates to the ability of plants and animals to withstand prolonged periods of desiccation. It has very high water retention capabilities and has the dual properties of both bioprotection and osmoprotection [89–94]. In vitro and in vivo studies have shown that trehalose protects corneal cells from desiccation [95], as well as protecting corneal and conjunctival cells against apoptosis [90,96]. Trehalose has also been shown to protect corneal cells against ultraviolet (UV)-induced oxidative damage by accelerating corneal healing [97], and reducing conjunctival inflammatory cytokines in a murine model of DED [92]. It also helps to restore osmotic balance to the ocular surface, as well as preventing denaturation of cell membrane lipid bilayers and proteins to maintain the homeostasis of corneal cells [90–92].
A new eye drop formulation that contains both HA and trehalose has been developed to capitalize on the lubricant properties of HA and bioprotectant properties of trehalose [98].
The presence of oxygen free radicals in the tears of patients with DED [99] has resulted in exploration of the potential application of antioxidants for the management of DED.
In an animal study, topical acetylcysteine, an amino acid with antioxidant activity, decreased inflammatory cytokine expression in ocular surface tissues of a mouse model of DED, but did not alter corneal staining [100]. Another antioxidant eye drop, vitamin A (retinyl palmitate), showed significant effects in improving blurred vision, TBUT, Schirmer score, and impression cytology findings in subjects with DED in a prospective, randomized, controlled, parallel study [101]. However, vitamin A metabolites are also known to cause MGD in animal models, including glandular keratinization and atrophy, reduced quality of meibum, reduced tear film break up time, increased tear film osmolarity, and dry eye symptoms (further details are included in the TFOS DEWS II Iatrogenic Dry Eye Report) [102].
A study using stratified human corneal limbal epithelial cells showed that several antioxidants may be beneficial if incorporated into topical ocular lubricants [103]. Quercetin, epigallocatechin gallate, n-propyl gallate, and gallic acid displayed good bioavailability, were effective at quenching reactive oxygen species and might be effective in protecting the corneal epithelium from oxidative damage.
Visomitin is the first registered drug with antioxidative properties that targets oxidative stress in mitochondria and is available as a topical drug in Russia. A recent multicenter, randomized, double-masked, placebo-controlled clinical study showed that a 6-week course of topical Visomitin reduced corneal staining and improved symptoms in 240 subjects with DED [104]. It may act through reducing reactive oxygen species on the ocular surface, but further studies are required to confirm this.
Selenoprotein P (SelP) is a secreted glycoprotein that is involved in the transport or storage of selenium, and is involved in oxidative stress metabolism [105]. In a rat dry eye model, the use of SelP eye drops for 3 weeks suppressed markers of oxidative stress and tears collected from human subjects with corneal staining were lower in SelP [106]. The authors concluded that tear SelP is a key molecule to protect the ocular surface against environmental oxidative stress.
Multidose artificial lubricants typically require a preservative to prevent microbial growth, whereas unit dose vials that are discarded after a single use do not. However, unit dose vials are more expensive and may be more difficult for less dextrous individuals to open. A number of new products are now available that utilise dispensers that incorporate unidirectional valves that allow multidose bottles to be unpreserved.
Increasing attention has been directed to the relationship between the chronic use of topical therapies, such as glaucoma medications, and OSD. Chronic exposure of the ocular surface to preservatives is now well recognized to induce toxicity and adverse changes to the ocular surface [107–112]. Benzalkonium chloride (BAK) is the most frequently used preservative in eye drop preparations. There are many in vitro and in vivo studies demonstrating that BAK can induce corneal and conjunctival epithelial cell apoptosis, damage the corneal nerves, delay corneal wound healing, interfere with tear film stability and cause loss of goblet cells [113–115]. In an in vitro study, a BAK concentration in excess of 0.005% significantly impaired lipid spreading and compromised the morphology of the tear lipid layer [116]. Sufficient evidence exists to confirm that patients with DED, particularly those with severe DED who require frequent dosing with lubricants or who use ocular lubricants in conjunction with other chronic topical therapies, such as glaucoma medications, should avoid the use of ocular lubricants preserved with BAK [102].
To avoid issues with long-term exposure to preservatives, newer variants of preservatives designed to have a lower impact on the ocular surface have been developed, including oxidative preservatives (sodium chlorite; Purite® and OcuPure™ and sodium perborate; GenAqua™), polyquaternium-1 (Polyquad®) and SofZia™. Sodium chlorite degrades to chloride ions and water upon exposure to UV light after instillation and sodium perborate is converted to water and oxygen on contact with the tear film. Some reports suggest that even these so-called “disappearing preservatives” can show some negative effects on the ocular surface [117]. Therefore, preservative-free drops may be a better choice for patients who have pre-existing ocular surface conditions and/or need frequent instillation of eye drops. Preservative-free eye drops have shown greater effectiveness than preserved drops in decreasing inflammation on the ocular surface and increasing the antioxidant contents in tears of patients with DED [118]. While ideally all prescribed dry eye products would be supplied in unit dose or unpreserved multi-dose bottles, cost considerations and product availability often prevent this from being possible.
Further information on preservative interactions with the ocular surface can be found in the TFOS DEWS II Iatrogenic Dry Eye Report [102].
The stability of commonly used ophthalmic solutions is controlled largely by the pH of their environment. In addition to stability, pH can influence comfort, safety, and activity of the product. Dry eye products contain a wide variety of buffers to control pH, including citrate, phosphate and borate buffers. The concentration of such buffers is critical, as reports exist of corneal calcification following extensive use of a dry eye product preserved with elevated levels of calcium phosphate [119].
Sodium borate, also known as sodium tetraborate or disodium tetraborate, is a salt of boric acid. Boric acid is a weak acid that is used as a buffering agent in some eye drops. Studies have shown that contact lens multipurpose solutions (MPS) containing boric acid may exhibit corneal epithelial cytotoxicity [120]. However, others have reported that MPS-induced ocular surface defects may be incorrectly attributed to boric acid [121]. The potential benefits, or otherwise, of boric acid or indeed any other buffers in dry eye formulations remain unclear. However, of note is that boric acid at ocular surface pH also acts as a cross-linking agent and electrostatically binds to hydroxypropyl guar (HP-guar) [122,123].
Due to the delicate structure of the ocular tissues, the number of acceptable excipients for eye drops is limited, and consists mainly of ionic and non-ionic isotonic agents. There are limited published studies concerning the effect of excipients on the ocular surface [124]. Recently, macrogolglycerol hydroxystearate 40 (MGH 40), has been used in preservative-free eye drops as a solubilizing excipient. An animal study showed that MGH 40 is well tolerated [125]. However, a prior in vitro study revealed that MGH 40 triggers similar detrimental effects in cells as that seen with BAK [126]. Another study examined the role of poly(L-lysine)-graft-poly(ethylene glycol) (PLL-g-PEG) as a novel polymer excipient in artificial tears [127]. A single-center study showed that PLL-g-PEG was effective in prolonging non-invasive break up time (NIBUT) 15 min after instillation [127]. More studies are needed to clarify the impact of the various excipients on the ocular surface.
The pre-corneal tear film is a complex milieu that is rich in electrolytes, including sodium, potassium, chlorine, magnesium and calcium [128]. When secreted, tears are isotonic with serum, although the proportions of ions are somewhat different, especially potassium [129,130]. In DED, the concentration of electrolytes in the tear film typically increases due to evaporation and/or reduced aqueous production.
Electrolytes perform critical roles in ocular surface homeostasis. Observations suggest that the relatively high potassium levels in tears may play a role in protecting the corneal epithelium from UV-B radiation [131,132]. Potassium has also been shown to be necessary to maintain normal corneal thickness, and decreases in the potassium concentration may result in an increase in corneal thickness [133]. Finally, the quality of the corneal epithelial surface integrity and light scattering properties, as measured by specular microscopy, have been shown to be dependent on electrolyte composition [134]. The epithelial surface is best maintained with a buffered solution containing potassium, calcium, magnesium, phosphate, bicarbonate and sodium chloride, with potassium being particularly important [134].
Certain tear lubricants, such as TheraTears® (Akorn Lake Forrest, IL, USA) and Bion® Tears (Alcon Ft Worth, TX, USA), have an electrolyte profile that is intended to reflect that of the tear film. Some of the commonly used electrolyte salts include sodium chloride, potassium chloride, calcium chloride, magnesium chloride, zinc chloride, sodium borate, sodium phosphate and boric acid. Sodium bicarbonate is used to buffer the solution, but also has an electrolyte effect [135]. An electrolyte-based artificial tear formulation has been shown to increase conjunctival goblet cell density and corneal glycogen content in a rabbit model of DED [58,59]. Other studies have shown that the inclusion of potassium with HA in non-preserved artificial tears enhances corneal wound healing in a mechanical scraping model [33]. The addition of bicarbonate to an isotonic, non-preserved artificial tear solution promotes recovery of the corneal epithelium compared with the same solution buffered with borate or without a buffer [136]. A separate study showed that addition of bicarbonate promoted recovery of epithelial barrier function and maintained normal corneal and mucin layer ultrastructure after exposure to BAK [137]. To date, in vitro, animal and human studies would suggest that certain electrolyte compositions could have a positive role in the management of DED with ocular lubricants.
The lipid layer of the tear film has an important role to play in preventing tear evaporation [138]. Lipid-containing eye drops are growing in both availability and popularity [139,140], primarily due to the increased attention being paid to MGD and lipid deficiency. A variety of oils, such as mineral oils and phospholipids, have been incorporated in ocular lubricant formulations to help restore the lipid layer of the tear film [46,141,142].
Lipid-containing drops are formulated as emulsions. Emulsions are defined as non-soluble liquids that are finely dispersed within another liquid, such as oil and water [143]. Emulsions are not readily formed and extreme shear forces and pressure must be applied with the appropriate surfactants to overcome the effects of surface tension [143].
Emulsions can be broadly categorized into three types, based upon the droplet size. Macroemulsions contain droplets larger than 100 nm (nm), nanoemulsions have droplets between 10 and 100 nm and microemulsions have droplets < 10 nm. Macroemulsions are cloudy because the large droplet sizes scatter light and these formulations can induce blur when applied topically. To minimize the potential blurring effect on vision, as well as the stability of the emulsion upon instillation, particle size, concentration and type of lipids can be manipulated. Smaller droplet sizes minimize blurring on installation because the droplet structures are smaller than visible wavelengths, which prevents scattering. A number of commercial products employ meta-stable emulsions to minimize blur time and therefore require the dispensing bottle to be inverted or shaken to enhance uniformity of the emulsion prior to application.
Emulsions have been demonstrated to effectively deliver lipophilic drugs, a task that is challenging for aqueous-based carriers. Newer approaches employ cationic submicron oil-in-water (o/w) vectors, which exploit the negative charges at the mucin layer [144]. A cationic o/w nanoemulsion is a biphasic formulation that comprises positively charged oil nanodroplets (the oil phase) dispersed in water (the continuous phase). The positive charge of the oil nanodroplets is brought about by a cationic surfactant that localizes itself at the oil interface. It is believed that when a cationic o/w nanoemulsion eye drop is instilled, the resultant electrostatic attraction between the positively charged oil nanodroplets and the negatively charged ocular surface mucins manifests itself macroscopically as an improved spreading and retention time [145]. It is possible that this interaction could be modified by exposure to cationic tear film proteins, such as lysozyme. This is of particular interest for patients with MGD who exhibit reduced tear film stability due to lipid deficiency within their tears [146].
Even in the absence of an active ingredient, these cationic o/w nanoemulsions have been observed in preclinical studies to have an inherent benefit on the ocular surface [147,148]. Cationorm® (Santen Osaka, Japan) is a preservative-free cationic emulsion indicated for the treatment of DED. The cationic excipient is cetalkonium chloride, an alkyl derivative of BAK that is lipophilic [148]. Some studies have shown that Cationorm is well tolerated by human corneal epithelial cells in culture [146,149]. However, another in vitro study demonstrated that corneas treated with Cationorm suffered epithelial loss and alterations to the superficial corneal stroma [150]. Cationic-based nanosystems incorporating chitosan provide alternative formulation strategies [151–153].
The long-term safety of nanoemulsions on the ocular surface remains to be evaluated.
Different types of lipids have been proposed to try to best mimic natural meibum. The types of lipids used include phospholipids, saturated and unsaturated fatty acids, and triglycerides [154]. Mineral oil in various concentrations, castor oil, olive oil, glycerin carbomers, coconut oil, soybean oil and lecithin, in combination with various emulsifying agents and surfactants, have been described [155–161].
Phospholipids can be neutral (zwitterionic), negatively (anionic) or positively (cationic) charged. Systane® Balance (Alcon Ft Worth, TX, USA) contains a polar phospholipid, DMPG (dimyristoylphosphatidylglycerol). Many types of phospholipids exist and, of these, two are commonly found in the tears - phosphatidylcholine and phosphatidylethanolamine [162–172]. It appears that anionic phospholipids have a greater ability to increase lipid layer thickness than zwitterionic compounds [46,173]. A possible reason is that negatively charged phospholipids contribute to a stable interface between non-polar lipids at the surface of the hydrophilic aqueous layer [174]. This supports a suggestion that polar phospholipids help to form a stable multi-molecular lipid film [175]. Studies suggest that lower levels of the two polar phospholipids are present in individuals with tear film deficiencies [165,176]. Further information can be obtained in the TFOS DEWS II Tear Film Report [128].
Multiple studies have shown that lipid-based drops and liposomal sprays can improve signs and symptoms of dry eye (Table 2) [65,141,142,177–182].
Serum is the fluid component of blood that remains after clotting. Although the topical use of autologous serum was described in the 1970's [183], it was only popularized for the management of severe OSD such as that associated with chemical burns, Stevens-Johnson syndrome and Sjögren syndrome many years later [184–186]. More recently, it has also been used for several less severe conditions, including post-laser epithelial keratomileusis (LASEK), recurrent corneal erosions, late onset bleb-leaks after trabeculectomy or tissue necrosis after orbital implants [187–189].
The advantage of autologous serum is that many of its biochemical characteristics, including pH, nutrient content, vitamins, fibronectin, growth factors such as epithelial growth factor (EGF) or nerve growth factor (NGF), are similar to that of human tears. Several in vitro and in vivo studies have shown that serum and other blood derivatives enhance corneal epithelial wound healing, probably due to these factors [190–194]. Serum was also found to inhibit the release of inflammatory cytokines and to increase the number of goblet cells and mucin expression in the conjunctiva in a clinical case series [195,196]. While evidence from cell cultures suggests that proliferation of epithelial cells is enhanced by diluting the serum to 20% or less, epithelial migration and extracellular matrix deposition from fibroblasts is better stimulated by 50% or 100% serum [197,198]. In a rabbit model, undiluted serum was more effective than diluted serum in healing a corneal epithelial wound [192].
The widespread use of autologous serum is limited by a number of factors. Production of blood products is regulated by national laws, which may differ significantly between countries. The process is frequently performed by blood banks and is centralised in some countries [199–201]. Legal requirements include serological testing for human immunodeficiency virus (HIV), hepatitis and other conditions, to minimize the risk of disease transmission during production or application by others, since unknown systemic infectious diseases have been observed in more than 3% of blood products [202]. The composition of the autologous serum obtained depends on a number of production parameters, including clotting or centrifugation time, and this is likely to have an impact on the epitheliotrophic effects [203]. To optimize the product and to permit comparison between studies, standardized protocols have been developed based on in vitro work, but these have not yet been confirmed in clinical comparative studies [204,205]. In addition to production issues, further issues exist around product storage, as the concentration of growth factors in autologous serum can reduce over time when stored at 4 °C [206]. At −20 °C the composition of autologous serum was found to be stable for up to 9 months [206–208]. Finally, the cost for autologous serum can prove to be problematic, as a 2–3 month supply can cost hundreds of dollars [205,209]. However, despite these issues, use of autologous serum in the management of severe OSD has gained widespread acceptance and thus may gain increased insurance-coverage in the future [210,211].
In a Level 3 study, autologous serum improved symptoms of dry eye within 10 days in approximately 60% of patients and within two months in 79% of patients [212]. This effect was sustained throughout a 12-month follow-up using various symptom questionnaires.
Table 3 presents the results from 14 clinical studies (Levels 1 & 2) on the efficacy of autologous serum in DED [184,186,213–224]. In these, 349 patients received autologous serum, predominantly for severe DED due to Sjögren syndrome. Between these studies there is substantial variation for production parameters, endpoints, dosing frequency and duration of treatment. In all of the trials, with a follow-up between 1 and 3 months, subjects showed significant improvement in symptoms, with 60–80% of patients showing a positive response. Typically, TBUT, corneal fluorescein staining and conjunctival impression cytology improved, while Schirmer scores remained unaltered.
Prospective comparative cohort studies showed that autologous serum was less effective in patients who were classified, historically, with secondary compared to primary Sjögren syndrome and that chronic OSD was more likely to recur after cessation of the autologous serum than acute OSD [184,186].
In a retrospective case control study (Level 2) of 16 patients with corneal neuropathy and photoallodynia (increased light sensitivity) associated with dry eye, in vivo confocal microscopy revealed a reduced sub-basal corneal nerve length and number [222]. Treatment with autologous serum for 3–4 months resulted in significantly decreased symptom severity and substantial improvements in a variety of nerve parameters. These findings support the positive effects reported for autologous serum in neurotrophic keratopathy in a clinical cohort of 42 subjects (Level 3) [225].
Although contamination of autologous serum is frequent after extended use (30 days) of dropper bottles, complications arising from contamination are generally rare [226–228]. However, the lack of a universally accepted methodology for the preparation of autologous serum and contamination concerns have hindered regulatory approval and limited its widespread adoption by clinicians. To overcome this, 100% autologous plasma from plasmapheresis, which minimizes contamination, has been proposed [229].
In summary, autologous serum contains specific epitheliotrophic factors such as EGF, NGF, and others, in addition to a high concentration of proteins such as albumin and fibronectin. Autologous serum directly supports the proliferation and migration of epithelial cells or indirectly enhances epithelial viability by binding and neutralizing inflammatory cytokines. The majority of clinical trials and case series studying autologous serum suggest that it can be effective in the management of OSD secondary to DED, probably due to its anti-inflammatory, epithelio- and neuro-trophic functions, significantly improving signs and symptoms within a few weeks. While the treatment is resource-intensive, it has few complications, but OSD can recur after cessation of treatment.
Concerns have been raised regarding the use of autologous serum when patients have active systemic inflammation, or fear of venipuncture, or in infants, the very elderly, or those with chronic anemia [230]. Allogeneic serum can be an alternative for these patients, and, as it can be prepared from previously stored blood, is quicker to produce and thus potentially more convenient. However, concerns remain in using allogeneic sources for proteins due to the theoretical risk of an immune response to foreign antigens.
Limited clinical data evaluating the role of allogeneic serum for the treatment of DED exists. In a series of 16 patients with graft versus host disease (GVHD), improvements in symptoms as measured by the OSDI, corneal fluorescein staining, TBUT, goblet cell density, and tear osmolarity were seen after treatment with 20% allogeneic serum eye drops prepared from the patient's spouse or related donors and used 6–8 times a day for 4 weeks [231]. Harritshoj and colleagues reported a series of 20 patients with DED due to GVHD, rheumatoid arthritis and other systemic immune diseases, and found that 16/20 (80%) of these patients showed improvements in objective signs and subjective symptoms of DED with 20% allogeneic serum treatment 6 times a day for 2–4 weeks [232]. These investigators used ABO specific male donors to exclude the risk of immune reactivity of ABO antibodies with ocular surface antigens. However, non-matched serum drops from mixed gender AB blood group donors have been used in New Zealand since 2007, with no reported adverse events [233]. To date, there have been no reports of significant complications associated with unmatched allogeneic serum, used topically, in the literature.
Umbilical cord serum has similar advantages to allogeneic serum, in that it can be prepared in large quantities (up to 250 ml) from a single donor and be used for many patients. Moreover, it is useful in patients with systemic inflammation, anemia or chronic diseases, who may not be ideal candidates for autologous serum drops. To prepare umbilical cord serum, umbilical cord blood is taken from the umbilical cord vein after delivery. After centrifugation, the serum is diluted to a 20% concentration and administered 4–6 times per day [234].
Umbilical cord serum has a higher concentration of tear components such as EGF, NGF and transforming growth factor (TGF)-β compared to peripheral blood serum [235]. Symptom scores, TBUT, corneal fluorescein staining and impression cytology findings have been shown to improve significantly after application of umbilical cord serum eye drops in patients with DED resistant to conventional treatment [235] and in ocular GVHD [236]. Comparison of umbilical cord serum with autologous serum administered 6–10 times a day showed that although both serum drops resulted in improvement, umbilical cord serum resulted in lower symptom and corneal fluorescein staining scores in severe DED and higher goblet cell density in Sjögren syndrome than did autologous serum [216], thought to be due to a higher concentration of growth factors and cytokines.
Platelets are a reservoir of biologically active growth factors. Hartwig and colleagues initially suggested the potential use of platelet preparations to treat ocular surface disorders [193,194]. Liu et al. compared the growth factor content of fresh frozen plasma and platelet releasate to that of serum and evaluated their effects on proliferation, migration and differentiation of corneal epithelial cells, in an in vitro system [237]. They found that the growth factor content was higher in platelet releasate than plasma or serum, with better cell proliferation, but that serum had better cellular migration and differentiation owing to its higher content of fibronectin and vitamins.
There are many different platelet preparations used in clinical studies, including platelet-rich plasma, plasma rich in growth factors and platelet lysate. These preparations differ widely in their method of processing [193,194,237–241].
In a prospective study, Alio and associates reported that the use of platelet-rich plasma 4–6 times a day in 18 patients with DED led to an improvement in symptoms in 89% and reduced corneal staining in 72% of patients after 1 month [242]. Plasma rich in growth factors, administered 4 times a day to 16 patients with DED, was found to be effective in reducing symptoms in 75% of patients after 3 months of treatment [243]. Platelet lysate (30%) applied 4 times a day was effective in a series of 23 patients with refractory GVHD, with improvement in corneal fluorescein staining in 70% of patients after 6 months of use [244]. Platelet Rich Plasma improves symptoms and signs of DED after laser in-situ keratomileusis (LASIK) [242]. However, the preparation is more complex and the beneficial effects and indications of using platelet-derived products over serum in the management of DED have not been addressed in the literature.
Mucolytics are a group of substances that depolymerize mucin and include ambroxol (Mucosolvan® Boehringer Ingelheim, Ingelheim am Rhein, Germany) and bromhexine that are used in the management of lung complaints that result in excess mucous production. A small clinical trial in subjects with Sjögren syndrome demonstrated that oral ambroxol improved dryness symptoms [245]. Another mucolytic eye drop, acetylcysteine, which also has antioxidant properties [246], has been reported to have a better effect in reducing subjective symptoms of DED than artificial tears, but had no effect on the objective signs [247]. In addition, mucolytics can be used for palliative treatment of filamentary keratitis, which is a potential complication of DED [248].
A transient receptor potential vanilloid type 1 (TRPV1) channel has been found in ocular surface tissue, which can be activated by hypertonicity to induce pain and inflammation [249,250]. Topical administration of SYL1001, a short interfering (si) RNA targeting TRPV1 (at a dose of 1.125% once a day), produced a significant decrease in symptom scores in subjects with DED compared with placebo [251]. Selective inhibition of the production of the TRPV1 receptor may reduce dry eye symptoms and may provide a novel therapeutic opportunity for the relief of dry eye, but further research is necessary to investigate this hypothesis.
The concept of temporary or permanent occlusion of one or both puncta is to retain tears on the ocular surface by blocking their drainage.
Any condition that would benefit from aqueous retention on the ocular surface is a reasonable indication for either unilateral [252], or bilateral, punctal occlusion [253]. These conditions include symptomatic contact lens wear [254,255], dry eye related to refractive surgery [256–258], ADDE secondary to a variety of systemic diseases (including Sjögren syndrome, GVHD, autoimmune diseases) [259,260], dry eye associated with a rapid TBUT [252], systemic medications that reduce tear film production, superior limbic keratoconjunctivitis [261], any corneal irregularities or scarring that affect tear stability, lid palsy or lid closure abnormalities, and toxic epitheliopathy [262].
The use of punctal occlusion in the presence of ocular surface inflammation is controversial, because theoretically occlusion of tear outflow could prolong the presence of pro-inflammatory cytokines on the ocular surface and treatment of the inflammation prior to occlusion is therefore recommended. However, a recent study showed that punctal occlusion in 29 individuals with moderate DED for 3 weeks resulted in reduced corneal fluorescein staining and symptom scores, without elevation of cytokine or matrix metalloproteinase (MMP)-9 levels, questioning whether cytokine levels would necessarily elevate with punctal occlusion over short periods of use [263].
Punctal occlusion is most commonly undertaken using punctal plugs. The plug can be located at the level of the punctal opening or deeper within the canaliculus. While it is relatively simple to understand the rationale for using punctal plugs for ADDE, its use in the management of EDE remains controversial and the results are equivocal as to its effectiveness in improving meibomian gland status and lipid layer instability [264–267].
Punctal plugs are differentiated into absorbable and non-absorbable devices.
Absorbable devices are temporary inserts that are typically used as “test” devices to determine the efficacy of occlusion, prior to permanent occlusion being undertaken. Collagen-based plugs, which absorb in one to 16 weeks, are the most commonly used [253,268,269]. Atelocollagen is a collagen solution that is extracted from animal dermal tissue, from which antigenic telopeptides attached to both ends of the collagen molecule are eliminated by pepsin treatment [270]. At temperatures of 4 °C or under, atelocollagen dissolves in a neutral phosphate buffer solution. If this solution is injected through the punctum, it turns into a white-colored gel at body temperature. The injectable atelocollagen plug has proven successful in a variety of studies [270–272]. Succinylated collagen plugs [273], and hypromellose 2% [274], may be promising alternatives for temporary punctal occlusion.
Non-absorbable or “permanent” plugs are often silicone-based and exist in a wide variety of designs. The Freeman style plug consists of a surface collar resting on the punctal opening, a neck, and a wide base, while the Herrick plug is a cone-shaped intracanalicular silicone plug [275]. Some silicone plugs have an interior channel for partial occlusion, which might permit limited drainage. The cylindrical SmartPlug™ is an intracanalicular plug made from a thermolabile polymer that changes size and shape when inserted into the punctum [276–279]. The FORM FIT® (Oasis Medical, Glendora, CA, USA) intracanalicular plug is made from an injectable hydrogel that hydrates in situ over a 10 min period and expands to conform to the shape of the canaliculus [280], removing the requirement for selecting a plug of the appropriate size. The plug is supplied on a pre-loaded inserter that dispenses the plug from within a polyamide sheath.
In addition to devices, certain types of cyanoacrylate adhesives can be used for temporary punctal occlusion, prior to determining if longer-term occlusion is warranted [281,282]. For permanent occlusion, there are a variety of surgical options that can be used, as described in section 2.2.1.3.
The most common complication of punctal occlusion is spontaneous plug extrusion [265,283–286], which may occur in as many as 60% of cases [287–289]. Other reported complications include infection [290–292], canalicular migration of the plug [286,290], pyogenic granuloma, punctal enlargement [286], and, rarely, tumors [293]. Infections (such as keratitis, conjunctivitis, canaliculitis or dacryocystitis) occur more commonly with intracanalicular devices [291,294]. Other less serious complications, frequently due to the mechanical presence of the device, include conjunctivitis, subconjunctival hemorrhage, chemosis, epiphora, punctal erythema, discomfort and foreign body sensation [294].
Permanent surgical closure of the punctum is typically reserved for patients who are unable to retain or tolerate punctal plugs. A wide variety of surgical methods exist [281], including total or partial thermal cauterization [295–298], punctal occlusion with a conjunctival flap [299] or graft [300], punctal plug suturing [301], total destruction (extirpation) of the canaliculus [302], and canalicular ligation [303]. The thermal methods include cautery, diathermy and use of an Argon laser, and these may be performed deep within the canaliculus or superficially on the external portion of the puncta [259,297,298]. Today, disposable, hand-held thermal cautery is the most widely used method in clinical practice.
There are currently no Level 1 studies and only a limited number of Level 2 reports regarding the efficacy of surgical closure of the puncta for treating DED. Comparative case series have demonstrated that permanent closure of the puncta by cauterization significantly improves symptoms, Schirmer scores, corneal fluorescein staining, rose bengal scores and TBUT in patients with GVHD and Stevens-Johnson syndrome [259,304].
Very few complications are reported with cauterization. Epiphora can be a potential problem if both the upper and lower puncta are totally and permanently closed. To avoid this, incomplete occlusion of the puncta can be achieved with thermal cautery. In patients with Sjögren syndrome, this partial occlusion technique has resulted in improved symptoms, TBUT, conjunctival staining and corneal fluorescein staining [298]. Recanalization can occur, depending on the technique used and the inflammatory response that occurs, and in such cases a repeat procedure is necessary to completely close the punctum [297]. It appears that techniques involving superficial cauterization have a higher rate of recanalization [305], and that deeper surgical procedures may increase the success rate [296].
Punctal occlusion may be most successful when combined with other DED treatments [306]. A systematic review of punctal occlusion for DED was conducted by Ervin et al., which included 7 studies with 305 subjects [307]. The author's conclusion was that, although punctal plugs provided symptomatic improvement and clinical outcomes improved from baseline measures, few studies demonstrated a benefit of punctal plugs over a comparison intervention. Further, these authors stated that although the evidence is very limited, the data suggest that silicone plugs can provide symptomatic relief in severe dry eye and that temporary collagen plugs appear similarly effective to silicone plugs on a short-term basis [307].
To date, there are no large scale, Level 1 studies to support the contention that punctal occlusion of any form is effective in the management of DED. However, 14 supportive Level 2 studies are listed in Table 4 [252,257,263,270,272,274,283,308–313].
Moisture chamber spectacles are eyeglasses specially designed to slow evaporation of the tears, by providing a humid environment and minimizing airflow over the ocular surface. A number of such devices are available. While the clinical efficacy of moisture chamber spectacles has been reported in case reports [314,315], to date, no high level studies have investigated the therapeutic value of these devices, but it does appear that they can prove to be a potential adjunct to prescribed treatment, especially in adverse environments [316].
Locally placed humidifying devices have also been proposed to enhance humidity or local air quality. However, only one controlled study lends support to their effectiveness in the management of dry eye thus far [317].
Several topical pharmacologic agents that stimulate aqueous, mucin and/or lipid secretion are commercially available in certain markets, or under development.
Diquafosol tetrasodium (Diquas®; Santen, Osaka, Japan) is approved as an ophthalmic solution at 3% concentration in Japan and South Korea for the treatment of dry eye. It is a purinergic P2Y2 receptor agonist that stimulates water and mucin secretion from conjunctival epithelial cells and goblet cells, leading to improved tear film stability in dry eye [14,318,319]. Several randomized controlled trials have demonstrated that the application of topical diquafosol significantly improves objective markers of DED, such as corneal and conjunctival fluorescein staining and, in some studies, TBUT and Schirmer scores [38,320,321]. Diquafosol has potential utility in various specific dry eye disorders, including Sjögren syndrome [322], ADDE [323], short TBUT dry eye [324], MGD [325], dry eye following LASIK [326], and cataract surgery [327], as well as in contact lens wearers [325]. Recently, Byun et al. demonstrated that diquafosol is effective in promoting corneal epithelial wound healing and that this effect may result from epidermal growth factor receptor/extracellular-signal-regulated kinase stimulated cell proliferation and migration via P2Y2 receptor mediated intracellular calcium elevation [328]. In studies in the USA, 2% diquafosol tetrasodium did not achieve its primary and secondary endpoints and failed to achieve FDA approval [329].
Lacritin is a glycoprotein that has prosecretory activity in the lacrimal gland and mitogenic activity at the corneal epithelium and is reduced in the tears of patients with Sjögren syndrome [330], and other forms of dry eye [128]. Topically administered lacritin has therapeutic potential for the treatment of ADDE [331].
There are a number of drugs that specifically target mucin deficiency in DED, including diquafosol tetrasodium (see section 2.3.1.1).
Rebamipide ophthalmic suspension (Mucosta®; Otsuka Pharmaceutical, Chiyoda, Japan) is currently approved in Japan for the treatment of dry eye. It is a mucin secretagogue that promotes the production of mucin-like glycoproteins in human corneal epithelial cells, increasing MUC1, MUC4 and MUC16 expression levels through signals involved in epidermal growth factor receptor activation [14,332]. In a multicenter, open-label, single-arm study, a total of 154 patients received 2% rebamipide four times per day for 52 weeks [333]. Lissamine green conjunctival staining, corneal fluorescein staining, TBUT and subjective symptoms improved significantly at week 2 compared with baseline, and further improvements were observed at every visit up to week 52. Topical rebamipide is also potentially effective in treating other ocular surface disorders such as short TBUT dry eye [334], lid wiper epitheliopathy [335], and alkali ocular damage [336,337]. Rebamipide has also proven to be effective at improving the ocular surface appearance and optical quality in patients with dry eye undergoing refractive surgery [338]. Although approved in Japan, phase III trials for rebamipide in the USA failed to provide the data necessary for FDA approval [329].
Galectin-3, a member of the lectin family, is a carbohydrate-binding protein that controls multiple biological processes within the epithelium of the ocular surface. It has been shown that individuals with DED have a higher concentration of galectin-3 protein in their tears compared with normals and it was concluded that the release of cellular galectin-3 into tears was associated with the development of epithelial damage [339]. The placental extract-derived dipeptide (JBP485), a dipeptide that promotes galectin-3 production, promotes the expression and secretion of the gel-forming mucin 5AC (MUC5AC) in rabbit conjunctival epithelium [340]. JBP485 has also been shown to elevate the expression of membrane-bound mucins (MUC1/4/16) in rabbit corneal epithelium. JBP485 induced tear secretion in the rabbit model and resulted in reduced corneal epithelial damage in a mouse dry eye model. Thus, JBP485 promoted both mucin and aqueous tear secretion improvements in animal models [340].
Mycophenolate mofetil (MMF) is a lymphocyte inhibitor commonly used in the treatment of autoimmune diseases and transplant rejection. It has been reported that a low concentration of MMF can promote human conjunctival goblet cell proliferation, and increase messenger RNA (mRNA) production of MUC5AC in vitro [341], but clinical studies are yet to be undertaken.
Eupatilin is a type of flavonoid. It has potent effects on inducing secretion of mucins in conjunctival cells, in both in vitro and in vivo studies, suggesting that it might have potential as a future treatment for DED [342,343].
Trefoil factors are secretory products of mucin-secreting cells. It has been found that the levels of Trefoil factor family peptide 3 (TFF3) are elevated in the tears of patients with DED. In an in vitro study, some proinflammatory cytokines, but not hyperosmolarity, were shown to also induce the production of TFF3, suggesting that TFF3 could be a potential target for the treatment of DED [344,345].
NGF regulates the growth, proliferation and maintenance of certain neurons. In an in vitro study, NGF was shown to stimulate conjunctival epithelial cell differentiation and mucin production [346].
Insulin-like growth factor 1 (IGF-1) has lipid-stimulating effects on meibomian gland cells in vitro [347]. Androgens have been found to upregulate genes involved in lipid metabolic pathways, and downregulate those related to keratinization, in human meibomian gland epithelial cells in a number of laboratory-based studies [348–351]. Phase 2 clinical trial results show that treatment of patients with MGD with topical testosterone improves the quality of meibomian gland secretions and reduces ocular discomfort [352]. Additional clinical trials for the treatment of MGD with topical testosterone are currently underway in Europe.
More details on the impact of androgens and IGF-1 can be found in the TFOS DEWS II Sex, Gender, and Hormones Report [353].
Two orally administered cholinergic agonists, pilocarpine and cevimeline, are commercially available for the treatment of Sjögren syndrome-associated DED. People with Sjögren syndrome have autoantibodies that bind to muscarinic acetylcholine receptors in the exocrine glands and pilocarpine and cevimeline are muscarinic acetylcholine receptor agonists (parasympathomimetics) that aim to overcome this effect.
People with Sjögren syndrome treated with oral pilocarpine for 12 weeks experienced a beneficial effect on symptoms and reduction in rose bengal staining, but an increase in tear production was not substantiated [354]. Other studies have shown an improvement in symptoms, corneal fluorescein staining, rose bengal staining, goblet cell density and TBUT, but again no improvement in tear production was shown by Schirmer testing [355,356]. However, oral pilocarpine was able to increase tear meniscus height (TMH) in people with Sjögren syndrome [357]. The most commonly reported side effect from this medication was excessive sweating, which occurred in up to 25% of patients [358].
Petrone et al. evaluated the safety and efficacy of 2 doses of cevimeline for the treatment of xerostomia and dry eye in patients with Sjögren syndrome in a 12-week double-masked, randomized, placebo-controlled study [359]. Patients taking cevimeline three times per day had significant improvements in subjective assessment of ocular dryness, dry mouth, and increased salivary and lacrimal flow rates [359]. Frequently reported adverse events included headache, increased sweating, abdominal pain, and nausea [359,360].
The efficacy of oral secretagogues seems to be greater in the treatment of oral dryness than ocular dryness [361,362]. Patients with Sjögren syndrome have been found to be more likely to continue cevimeline than pilocarpine on a long-term basis due to fewer reported side effects with cevimeline. Therapeutic failure of one secretagogue did not predict similar results with the other, with second time users more likely to continue long-term treatment [358].
Neuromodulation is a therapeutic strategy that involves interfacing directly with the nervous system through electrical, electromagnetic, chemical, or optogenetic methodologies [363,364]. The goal is the long-term activation, inhibition, modification, and/or regulation of neural input to correct organ or tissue dysfunction and manage disease symptoms. The nasolacrimal reflex upregulates tear production following chemical or mechanical stimulation of the nasal mucosa [365,366]. The nasolacrimal reflex arc begins in the sensory nerves lining the nasal cavity (the afferent arm) and terminates with the parasympathetic innervation of key target tissues that contribute to tear production (the efferent arm) [367]. In a prospective, case-control study in patients with normal tear production, anesthetizing the nasal mucosa was shown to reduce basal tearing by 34% compared with a saline control [368].
An intranasal tear neurostimulator has been developed to induce normal tear production via stimulation of the nasolacrimal reflex. This device consists of a hand-held stimulator unit equipped with a disposable two-pronged hydrogel tip and an external charger. The intranasal tear neurostimulator allows self-delivery of minute electrical currents to the anterior ethmoidal nerve, thereby stimulating immediate natural tear production in patients with DED [366]. Forty subjects with mild-to-severe DED used a prototype intranasal tear neurostimulator in an open-label, single-arm, non-randomized, 180-day pilot study [369]. Subjects were instructed to perform stimulation with the device 2 times per day or more, as needed. At day 180, stimulation with the device significantly increased mean Schirmer scores compared to unstimulated basal tear production scores. At the end of the follow-up period, mean conjunctival staining and symptom scores were significantly reduced from baseline. Preliminary results have also shown a positive effect of the neurostimulator on goblet cell function [370].
The TrueTear™ Intranasal Tear Neurostimulator (Allergan, Parkway Parsippany, NJ, USA) was recently cleared by the FDA with an approved indication for providing a temporary increase in tear production during neurostimulation in adult patients. A number of other studies are ongoing and results are awaiting publication [371,372].
A variety of other novel methods to stimulate tear production have been reported. These include abdominal breathing for 3 min, which reportedly increased the tear meniscus volume in healthy women [373].
Corneal cold thermoreceptors are activated by drying of the ocular surface and stimulation of these receptors could increase tear production [374,375]. The existence of Transient Receptor Potential Cation Channel, Subfamily M, Member 8 (TRPM8) on the nerve terminals of the cold thermoreceptors on the cornea is consistent with the finding that their stimulation by menthol and cool temperatures could increase tear production [376,377]. Finally, caffeine, probably the most widely consumed psychoactive substance, appears to stimulate tear secretion in healthy, non-dry eye subjects [378].
Appropriate lid hygiene is important in the management of a variety of lid conditions that result in dry eye (particularly blepharitis) and, if used appropriately, can reduce lipid by-products and lipolytic bacteria associated with these conditions [379–385]. Lid scrubs using a mild dilution of baby shampoo applied with a swab or cotton bud have been the most widely accepted therapy [382,386,387]. A recent Level 1 study demonstrated the efficacy of lid scrubs for removal of crusting in anterior blepharitis, with both a commercial lid cleanser and dilute baby shampoo [388]. However, relative to the baby shampoo, the dedicated lid cleanser showed reduced ocular surface MMP-9 levels, improved lipid layer quality and was better tolerated. Baby shampoo was further reported to be associated with a reduction in ocular surface MUC5AC levels, suggesting that baby shampoo may have an adverse effect on goblet cell function [388]. In preference to using baby shampoo, there are now a wide variety of proprietary lid cleansing products available, which utilise a diversity of delivery mechanisms, including scrubs, foams, solutions, and wipes; their individual description is outside the scope of this review.
The report of the TFOS MGD Workshop reported that “lid hygiene is widely considered an effective mainstream therapy for MGD and blepharitis” [389]. However, compliance with following lid hygiene instruction is notoriously poor. A recent cross-sectional study of 207 subjects who were prescribed lid hygiene procedures (daily warm compresses and eyelid scrubs) found that only 55% were compliant after 6 weeks of use [390].
Despite the fact that various professional organisations suggest ways to clean the eyelids, to date, there are no universally accepted guidelines for lid cleansing and peer-reviewed evidence for such advice is lacking, suggesting that this is an area worthy of study. Caution should be exercised when cleaning lids that have make-up on them, to avoid subsequent contamination of the ocular surface [391–393].
Table 5 reports Level 2 studies related to lid cleansing methods and their impact on blepharitis or dry eye (combinations with other pharmacological treatments are not included) [386,387,394–400].
Lid hygiene to reduce the bacterial load on the lid margin is commonly undertaken in the management of DED associated with blepharitis [401]. However, achieving this through prescribing topical antibiotic drops or ointment (such as fusidic acid) alone is not commonly recommended over the longer term, but is adopted by some practitioners [402] and a short dose of a topical antibiotic has been recommended in consensus-based reports [403]. A recent Level 2 study demonstrated that an ofloxacin-based ointment was valuable in the management of patients with obstructive MGD. Topical azithromycin (a macrolide antibiotic) has been used in the management of DED, but it is believed to have an anti-inflammatory action rather than simply reducing the bacteria lid flora (see Section 4.5). More Level 1 studies are required to examine the potential for prescribing topical antibiotics alone in managing DED.
Demodex infestation is a causative factor in many cases of intractable blepharitis and is often associated with dry eye symptoms [404], although there is currently no evidence to show a direct association with the development of MGD [389]. Historically, the treatment of ocular Demodex included a wide variety of products, most of which had no high level evidence to support their use. These included topical 2% metronidazole gel [405,406], 1% mercury oxide ointment [407], and 4% pilocarpine gel [408]. More recently, appropriate management has been found with the use of topical products containing tea-tree oil or oral ivermectin, as summarized in Table 6 [409–415].
Tea tree oil (TTO) is a natural, essential oil from steamed Melaleuca alternifolia leaves (from the narrow-leaved Paperbark or Tea tree, which is native to Australia) that exhibits antimicrobial, anti-inflammatory, antifungal, and antiviral properties [416], and is toxic to Demodex [417]. In a Level 2 clinical study, a weekly lid scrub with 50% TTO accompanied by a daily lid scrub with tea tree shampoo was more effective at eradicating ocular Demodex than a daily lid scrub with a 50% concentration of baby shampoo [417]. However, TTO can be toxic to the eye and causes ocular stinging and irritation if used in its pure form. The active component of TTO is 4-Terpineol [418,419], and pre-formulated wipes are now commercially available that are equivalent to 25% whole TTO. These reduce the risk of toxicity to the ocular surface compared with using stronger concentrations of TTO. Several studies have shown a considerable reduction in the number of Demodex on the eyelashes after treatment with TTO [409,410,413,414,417].
To date, very limited information exists in relation to the positive impact of TTO on dry eye symptoms and signs [420], and more studies are needed on this topic.
Ivermectin is a broad-spectrum antiparasitic drug primarily used to treat strongyloidiasis and control onchocerciasis. It is a low cost, single dose medication that is very well tolerated by patients. One oral dose of ivermectin has been shown to successfully reduce the number of Demodex found adjacent to the lashes of patients with blepharitis [411,412]. Performance has been improved by combining the use of ivermectin with metronidazole [415], or with permethrin cream [421]. More studies are needed to confirm the role of ivermectin for treating DED symptoms and signs.
The 2011 definition of MGD by the TFOS MGD Workshop highlighted the importance of terminal duct obstruction in MGD [2], which has encouraged the use of treatments to remove obstruction from the terminal duct and ductal system of the meibomian glands. Thus, there exists a significant role for conventional treatments in the management of MGD, including ocular lubricants, lid hygiene and warm compresses.
As MGD results in decreased lipid layer thickness, it may be beneficial to replace the lipids with ocular lubricant eye drops or sprays that contain lipids. A number of studies have found an improvement in signs and symptoms with the use of lipid-based drops in dry eye (Table 7) [65,141,142,157,182,422–427]. A Level 1 study has confirmed increased lipid layer thickness grade and NIBUT in normal eyes treated with a liposomal spray [178]. To enhance the potential performance of lipid-based drops, nano-technology concepts have been incorporated into lipid emulsion eye drops [147,428].
Despite the proven efficacy of warm compresses in many clinical studies, compliance is often poor due to the time required and the difficulty in maintaining the temperature of the compress for an extended period of time [389,390,429–432]. One method to extend the length of time over which a facecloth can retain heat is to wrap several cloths around each other in a bundle format [433].
The ability for heat from a warm compress to soften or liquefy the secretions in obstructed glands in the case of MGD is supported by Level 2 and 3 evidence [433–436]. The temperature and time required for melting obstructive material within the meibomian gland excretory duct has not been definitively established. Preliminary evidence from multiple studies has reported a range of melting points (32°-45 °C) for the contents of the meibomian glands, reflecting in part that meibum is a highly complex lipid mixture [434,435,437–439]. Meibomian gland material causing severe obstruction has a higher melting point than material from less obstructed glands [434,437,440]. Level 2 and 3 evidence suggests that heating the individual meibomian gland to a temperature of ≥40°C is likely to be required for optimal warm compress treatment [433,437,441]. The 40°C recommendation refers to the temperature of the palpebral conjunctiva and the gland, not the temperature on the contact surface of the treatment device or the temperature of the external skin of the eyelids.
Arita and colleagues evaluated the impact of 5 commercially available eyelid-warming devices in 10 subjects with MGD and 10 controls over a 2–4 week period [442]. The 5 devices consisted of 2 dry (non-moist) methods and 3 moist methods. A single application of all 5 devices improved symptom scores, increased TBUT and increased ocular surface temperatures, but only for up to 30 min. The moist devices resulted in “wetness” of the surface of the eyelid skin, resulting in evaporative cooling that tended to limit the beneficial effects of lid warming. Their results showed that repeated eyelid warming with a non-moist device improved tear film function in normal individuals and may have beneficial effects on both tear film and meibomian gland function in MGD patients. They concluded that repeated non-moist warming for 2 weeks or 4 weeks was required to achieve a stable improvement in normals and in those with MGD respectively [442].
A prospective, randomized, contralateral eye study recommended that warm compresses, heated to 45 °C, should be applied to the outer lid for a minimum of 5 min. Optimal contact between the compress and eyelid should be achieved and the compresses should be replaced every 2 min to ensure the temperature is maintained [443]. Several preliminary studies on non-dry eye participants have investigated the effect of different warm compresses on eyelid temperature [433,444]. All of the compresses showed an increase in temperature at the lower lid conjunctival surface and none caused any damage to the eyelids. However, only the continuous layered application of warm bundled towels heated in a microwave was able to maintain a temperature of 40 °C on the lower lid conjunctival surface [433]. This study concluded that a wet surface improved heat transmission through the lid and should be used versus dry treatments [433]. Care should be taken not to heat the eyelid skin to more than 45 °C to avoid thermal damage [445,446]. Fortunately, a safeguard is the individual's pain response, that protects against extensive thermal damage to the eyelid skin as a patient will not tolerate a cloth that is excessively hot [447].
Of possible concern is the heating of the cornea from approximately 36 °C to 39.4 °C after approximately 8 min [448]. If eye rubbing occurs when the corneal temperature is elevated, corneal deformation and visual blur can result [449]. The risks of ocular massage with elevated corneal temperature have been deemed to require patient instruction on how to optimally perform the procedure [448,450].
A study of subjects with MGD showed that 12 weeks of lid warming therapy resulted in a therapeutic benefit, with excess ocular surface phospholipase activity (which is detrimental to tear film stability) being reduced [451].
In addition to homemade compresses, a wide variety of devices are now commercially available for the management of lid anomalies that will raise the lid temperature for a longer period of time [431,432].
Blephasteam® (Thea Pharmaceuticals, Newcastle under Lyme, UK) resembles a swimming goggle and is plugged into an electrical outlet to provide latent heat, without pressure, on the eyelids. A moistened insert is placed into each sealed watertight chamber to provide a warm, high humidity environment over each eye. A preliminary study on normal subjects found that the device increased the temperature of the eyelids [433], and a study on dry eye patients reported that tear film evaporation was reduced 32% immediately after treatment [452]. Two randomized, controlled, investigator-masked studies found greater efficacy with Blephasteam® than with warm towel treatment [429,453] and a randomized, investigator-masked, crossover study conducted on healthy volunteers found Blephasteam® warmed the lower eyelid for a significantly longer period of time than warm compresses [453]. Visual acuity also significantly improved after use of Blephasteam® [453]. Two prospective, non-randomized studies found improved symptoms in patients with MGD [430,454] and increased TBUT. Decreased acinar diameter and area were also observed in individuals unresponsive to warm compress treatment [430].
3.2.2.2 MGDRx EyeBag®
The MGDRx EyeBag® (The EyeBag Company, West Yorkshire, UK) is a reusable warm compress, consisting of a cotton and silk bag containing flax seeds, that is heated in a microwave for 30 s. Studies conducted in normal eyes found the MGDRx EyeBag® achieved higher ocular temperatures than another heating mask [455], and also maintains heat longer than a simple heated face cloth in both in vitro and in vivo studies [431,432]. A randomized, investigator-masked, contralateral study reported an improvement in symptoms after using MGDRx EyeBag® twice a day for two weeks [456]. The benefits lasted for up to 6 months, with occasional retreatment sessions leading to greater comfort.
3.2.2.3 EyeGiene® mask
The EyeGiene® mask (Eyedetec Medical, Danville, CA, USA) uses disposable pressure-activated warming units [455]. A randomized, controlled, examiner-masked study found the EyeGiene® mask was similar in efficacy to a warm towel, but not as effective as Blephasteam® [429] or as effective in raising ocular temperature as a flaxseed-based eye mask [457].
The infrared warm compression device consists of an eye mask with two rigid patches over the eyes. Each patch has 19 light emitting diodes, emitting near infrared radiation from 850 to 1050 nm, with a peak at 940 nm. The infrared warm compression device was used to treat 37 subjects with obstructive MGD in a prospective, non-comparative interventional case series for 5 min, twice a day, for 2 weeks with closed eyelids. Total subjective symptom scores improved and there was also significant improvement in tear evaporation rates during forced blinking, fluorescein and rose bengal staining and meibomian gland orifice obstruction score [458].
The purpose of applying physical treatment to the meibomian glands is to improve and/or restore the function of the glands by ameliorating or removing ductal obstruction, thus allowing the glands to become functional [459]. Physical expression for therapeutic amelioration of obstructive material should not be confused with diagnostic expression, where minimal forces are used to determine if the gland is functional [441].
There are three established methods for physically treating ductal obstruction; warm compresses and various heating devices use heat to raise the temperature to soften or preferably liquefy the obstructive material, physical force is used to compress the glands to physically express the material from the obstructed gland, and intraductal probing introduces a thin wire into the obstructed orifice and then uses force to expel the obstructive material.
There is a long history describing a variety of methods for forceful expression of the meibomian glands without the application of heat [460–462]. These methods include isolating the eyelid to be expressed between the examiner's fingers and applying force by squeezing the eyelids against each other, or utilizing a rigid object on the inner surface of the eyelid and the thumb or finger or another rigid object on the outer lid to apply force [460,463]. However, a limiting factor with all these methods is pain experienced by the patient, which is only minimally relieved by topical anesthetics. The amount of pain increases rapidly as the force of expression exceeds 5 pounds per square inch (PSI) [464]. The usual maximal tolerable force is 15 PSI, which is frequently marginal or inadequate to express obstructive material [464].
A study investigated the efficacy of four in-office forceful expressions over a period of 6 months in conjunction with daily warm compress therapy [461]. The number of expressible glands, quality of secretion and lipid layer thickness significantly improved and all patients reported improved comfort and decreased symptoms associated with DED [461].
LipiFlow® TearScience, Morrisville, NC, USA) was designed to bypass the impediments to heat transfer through the eyelid tissue and simultaneously evacuate the gland contents, while heating the glands to therapeutic levels of 42.5 °C [459,465]. It has been demonstrated, in both randomized controlled and uncontrolled clinical trials, that the single 12-min procedure of the LipiFlow® system is safe and effective for treating MGD and that the effect can be sustained [465]. The first prospective, open-label, randomized, crossover, multicenter study compared a single LipiFlow® treatment to daily warm compress therapy [459]. The group undergoing LipiFlow® treatment showed a significant improvement in symptoms, meibomian gland secretion and TBUT at one month, while the warm compress group showed improvement only in symptoms. After receiving the crossover treatment, the warm compress group also demonstrated significant improvement in gland function and TBUT.
More recently, a prospective, randomized, crossover, observer-masked clinical trial, compared a single LipiFlow® treatment to a robust 3 month regime of twice-daily warm compresses combined with both lid massage and lid hygiene [72]. These subjects were evaluated for six months, demonstrating that a single LipiFlow® treatment performs at least as well as the rigorous twice-daily hygiene, heat and massage regime and that the effects of the single LipiFlow® treatment were sustained for six months [466]. A more recent prospective, multicentre, open-label 12 month clinical trial randomized 200 subjects (400 eyes) and reported that the single LipiFlow® treatment effect, with improved gland function and dry eye symptoms, can be sustained for up to 12 months [467]. An uncontrolled single center, observational study found significant and sustained improvement in meibomian gland function and symptoms for up to 3 years after a single treatment [468].
Intense pulsed light (IPL) has been used in dermatology to deliver intense pulses of non-coherent light from 500 nm to 1200 nm in wavelength to treat various conditions, including skin pigmentation, sun damage and acne [469]. A hand held computer-controlled flashgun delivers the appropriate light, which is filtered for specific action.
IPL was first reported anecdotally over 15 years ago for the treatment of MGD. A more recent prospective, double-masked, placebo-controlled, paired-eye study compared the effect of multiple pulses of IPL on one eye while the other eye received a sham treatment. The treatment imparted an improvement in tear film quality and a reduction in symptoms [470]. A retrospective analysis of medical records has independently shown a 77% improvement in meibomian gland function in at least one eye and an 89% improvement in dry eye symptoms when IPL was used in combination with manual meibomian gland expression [471]. A retrospective multicentre cohort review of 100 patients with MGD treated with IPL showed similar clinical improvements and concluded that IPL therapy was a safe and effective treatment for EDE [472].
Intraductal meibomian gland probing was first described in 2010 [473]. This initial publication reported data from a retrospective chart review of 25 consecutive patients who all had signs and symptoms of obstructive MGD. Immediate post-probing relief was experienced by 24 of the 25 patients and all patients had relief from symptoms by 4 weeks after the procedure. Five patients required one or two retreatment sessions. The patients who underwent a single treatment were followed up on average at 11.5 months post treatment. All of the patients were symptom free at their last follow-up visit [473]. A prospective, longitudinal study performed probing on one eye of 16 individuals presenting with MGD, while the fellow eye was used as a control. Break-up time, vision, pain and photophobia all improved at one week and 6 months post-treatment [474]. A study of three patients with refractory obstructive MGD investigated the amount and change in meibum viscosity after probing. All patients showed improvements in lipid levels and viscosity and 2 of the 3 showed improved TBUT [475]. A study also reported improvement in symptoms after probing for 10 patients with ocular rosacea, MGD, and surface disease refractory to conventional management. Symptoms improved in approximately 50% of subjects at 1 and 6 months, doxycycline was discontinued in 9 of 10 patients and all patients reported decreased use of ocular lubricants [476].
While further research is indicated, especially in view of the invasive nature of the procedure, the possibility of damage to a complex ductal system and the small sample of subjects thus far reported on, the data reported suggest that intraductal probing may offer relief to MGD patients who are unresponsive to conventional treatment.
One of the primary mechanisms driving obstruction of the meibomian glands is hyperkeratinization of the eyelid margin and duct orifices [477]. As keratinized material is built up around and within the orifice, the gland is obstructed and meibum cannot be delivered from the gland to the tear film. Debridement of the line of Marx, which marks the mucocutaneous junction and the keratinized lid margin, was first reported in 2013 [478]. It is believed that this technique works by mechanically removing accumulated debris and keratinized cells from the eyelid margin to allow increased flow of meibum into the tear film. The prospective, investigator-masked study by Korb and colleagues included a test group of 16 subjects and a control group of 12 subjects, all presenting with symptoms of dry eye and visible changes to the line of Marx [478]. The stained line of Marx and the entire width of the keratinized lower lid margin were debrided in the test group using a stainless steel golf spud. One month post-treatment, significant improvements in symptoms occurred in 22% of subjects and in MG function occurred in 46% of subjects [478]. A prospective, randomized, unmasked, controlled pilot study to determine the effect of lid debridement in subjects with Sjögren syndrome was recently published [479]. All 14 subjects were female, seven were randomized to the treatment group and seven were controls. One month after debridement scaling subjects reported improved symptoms, ocular staining was reduced, and re-establishment of meibomian gland function was demonstrated [479].
A lack of sham treatment and masking in both reported studies [478,479] must be considered. Larger studies and additional study designs are needed to confirm the mechanisms of action to explain the positive results reported to date.
Incomplete blinking or an inability to close the eyes fully during sleep can result in drying of the ocular surface [480–482], and thus appropriate measures to address any blink or lid closure abnormalities are worthy of consideration in the management of the patient with signs or symptoms of DED.
Further details on the impact of abnormal blink patterns and eye closure on DED are detailed in the TFOS DEWS II Pathophysiology Report [483].
Studies investigating treatments for any form of inadequate lid closure are mostly Level 3 [481,484–487], and include the evaluation of tear supplements, ointments (typically instilled at night), moisture goggles, night time eyeshields that achieve mechanical closure of the lids, and forced temporary closure of the lids by patching or taping. For those unwilling or unable to perform eyelid physical taping overnight, such as those with contact dermatitis or those concerned with iatrogenic lash epilation [481,484], alternative methods exist. These methods include eyecups of a variety of different designs and materials, and the use of thin polymer films (such as plastic food wrap). Level 1 evidence suggests that films provide better protection to the exposed cornea, with fewer complications, than lubricants [488]. Mechanical closure of the eyelids by various methods in critically ill populations is reported to equally, or better, protect the exposed cornea, with fewer complications, than lubricants [488,489]. However, although it is universally accepted that mechanical closure of the eyelids is mandatory in the management of severe exposure keratopathy, there are no randomized prospective controlled clinical studies to establish the efficacy or superiority of different treatments.
Persistent or severe cases of corneal exposure may require one of a variety of surgical procedures, including implantation of upper lid weights [481,490,491], lid springs, lid reconstruction or partial/complete tarsorrhaphy. Rigid gas permeable scleral lenses can also be an option in cases of exposure keratitis, as detailed in section 3.3.3.2.
Entropion and ectropion result in ocular surface exposure and entropion often results in concurrent trichiasis, causing symptoms of dry eye [492]. Facial nerve palsy results in a paralytic lower lid ectropion and upper eyelid retraction due to reduced activity of the orbicularis oculi. Other causes include trauma, tumors, facial surgery and age-related lid laxity.
Management of both entropion and ectropion is usually surgical and techniques include tightening the canthal tendons and removing a cicatrix or other mechanical reason for eyelid malposition [493–497]. In a Level 2 study, correction of entropion improved vision, punctate keratopathy and TBUT, but not Schirmer results [498]. A further Level 2 study showed that tarsorrhaphy was a successful procedure for entropion and supported epithelial healing in severely dry eyes [499].
Contact lens use for the correction of refractive error in healthy eyes may be accompanied by symptoms of dryness and discomfort and the options to manage such discomfort have been addressed in detail elsewhere [500]. Despite their association with dryness, contact lenses have a potential role in the management of DED. In the framework of the original TFOS DEWS report, contact lens use was listed with permanent punctal occlusion and serum tears as options for more advanced DED [1]. The main reason that contact lens wear was reserved for management of more severe forms of DED is to acknowledge that OSD and contact lens wear are each risk factors for microbial keratitis, although the compounded risk factor is unknown. The mechanism by which contact lens wear is therapeutic has yet to be elaborated in detail, but relevant aspects include mechanical protection and reduction in corneal desiccation.
The decision to use a contact lens in the therapeutic management of DED must take into consideration the risks and benefits of the individual case. Reports of microbial keratitis occurring in patients fitted with contact lenses in the management of OSD have emerged [501], including cases that progressed to endophthalmitis [502]. Contact lenses worn for severe DED are often used on an extended wear basis, which is associated with an increased risk of microbial keratitis relative to daily wear [503–506].
The management of DED can be undertaken with either soft or rigid lenses. Depending upon the severity and nature of the OSD, therapeutic soft contact lenses, which are often termed bandage contact lenses, can be prescribed for short-term (days) or long-term (years) use and may be worn on either a daily wear or extended wear schedule.
The purpose of a bandage contact lens is to improve ocular comfort and reduce the effects of an adverse environment. The availability of silicone hydrogel soft lens materials, with high oxygen transmissibility, has encouraged the application of these devices for the therapeutic management of OSD, and they are typically used on an extended wear basis [507].
Bandage contact lenses are considered a useful adjunctive management option for a range of ocular surface pathologies, including recurrent corneal erosion [508], corneal abrasion [509], bullous keratopathy [510], and after corneal surgery [511–514]. It has been suggested that bandage contact lenses may stabilize the tear film and assist with the restoration of epithelial cell turnover [515], and potentially aid in the management of corneal pain by insulating sensitized corneal nerves from environmental stimulation [516,517]. The exact mechanism by which a bandage soft lens relieves pain has not been elucidated, but likely involves direct shielding of nociceptors at the ocular surface or support of cellular structure and extracellular matrix elements that serve a shielding role. A protective effect may arise in preventing drying or cooling of the ocular surface or in shielding the ocular surface nociceptors from lid and tarsal conjunctival related trauma, for example in cicatrising disease. The use of soft bandage contact lenses for DED is supported by Level 3 evidence that pain relief with bandage soft contact lenses can be achieved in corneal diseases other than DED [518], for example, when there is nociceptive pain after trauma and surgery [519].
There is currently a relative dearth of literature relating to the specific application of bandage contact lenses for the management of DED. A recent prospective, randomized (Level 1) study of 40 subjects with Sjögren syndrome that compared the efficacy of bandage contact lenses to autologous serum concluded that silicone hydrogel contact lenses (worn as a bandage contact lens), were effective in the management of Sjögren syndrome-associated DED [223]. After six weeks, subjects fitted with bandage contact lenses had a significant improvement in best-corrected visual acuity (which remained stable for up to six weeks after discontinuing contact lens wear) and significantly improved OSDI scores, compared with subjects treated with autologous serum. Both intervention groups also showed relative improvements in quality of life scores, tear break-up time and corneal staining, compared with baseline; there were no adverse events observed in either group. Furthermore, in a Level 2 study involving seven patients with GVHD and moderate to severe DED, the use of silicone hydrogel lenses, worn on a seven-night continuous wear basis for one month, was found to reduce dry eye symptoms and improve visual acuity compared with pre-treatment [515].
Timely treatment of any corneal epitheliopathy is considered important for minimizing the risk of developing chronic pain; once there has been centralization of neuropathic pain, a bandage contact lens, which might reduce peripheral signalling, may be insufficient for reducing symptoms [516].
There is increasing appreciation that daily wear of a rigid gas permeable scleral lens may play an important role in the management of moderate to severe DED, possibly due to the fact that they can provide a repository of tears between the lens and the ocular surface. The use of scleral lenses has been investigated in other conditions such as chronic GVHD [520–522], and Stevens-Johnson syndrome [523]. Use of a scleral lens as a prosthetic device in a series of patients, including those with OSD, was first reported from the United States in 1990 [524], with similar reports emerging from around the world that same decade [525,526]. A case series (Level 3 evidence) has described the long-term application of scleral contact lenses as an alternative to tarsorrhaphy in three patients who had developed unilateral lagophthalmos and corneal anesthesia secondary to post-surgical facial nerve paralysis [527]. The scleral lens modality was reported to provide effective protection to the ocular surface and optimize visual function in these patients. The use of scleral lenses for OSD is more widely reported in a variety of reviews [528–530].
Recent clinical studies report success in the management of DED with scleral lenses, mini-scleral lenses and PROSE (Prosthetic Replacement of the Ocular Surface Ecosystem) [520,522,527,531–538].
Corticosteroids are successfully used in the treatment of a wide range of inflammatory diseases, including DED.
Desiccating stress can induce ocular surface damage and generate innate and adaptive immune responses. These inflammatory cascades lead to further ocular surface damage and the development of a self-perpetuating inflammatory cycle. Inflammation can also cause alterations to the neurobiology of the ocular surface, as described in the TFOS DEWS II Pain and Sensation Report [539].
Steroids have been found to be useful in neural pain modulation, which may be beneficial in managing neuropathic pain, but this modulation has not been evaluated in the eye [540]. It is clear from numerous experimental studies in animal models that topical corticosteroids are effective in breaking the vicious cycle of immune responses in DED. Topical methylprednisolone (1%) treatment suppressed MMP-9 and inflammatory cytokine expression and mitogen-activated protein kinase activation in the corneal epithelium of experimental murine dry eye. As a result, desquamation of apical corneal epithelial cells was decreased and the integrity of corneal epithelial tight junctions was maintained [541,542]. In DED induced by intralacrimal gland injection of botulinum toxin-B in a mouse model, topical 0.1% fluorometholone alone or in combination with cyclosporine A, was able to partially restore tear production and significantly improve the ocular surface [543]. Murine studies have explored new therapeutic agents for DED. One study showed that a significant decrease in corneal fluorescein staining was observed after topical treatment with 1% methylprednisolone, 5% interleukin (IL)-1R antagonist, and 0.05% cyclosporine A [544]. A significant decrease in the numbers of central corneal CD11b+ cells, corneal lymphatic growth, and corneal IL-1β expression were also demonstrated after treatment with IL-1R antagonist and methylprednisolone, which were not observed after treatment with the vehicle [544].
Selective glucocorticoid receptor agonists can also be used as a therapeutic target for DED. In the atropine-induced dry eye rabbit model, selective glucocorticoid receptor agonists and 0.1% dexamethasone were fully efficacious, maintaining tear volume and breakup time [545]. Both agents showed no effects on intraocular pressure (IOP) or body weight, whereas dexamethasone significantly increased IOP and inhibited the increase of body weight due to muscle wasting [545]. Furthermore, selective cyclooxygenase-2/eicosanoid-prostanoid receptor (COX-2/EP receptor) inhibition is suggested as a therapeutic target in a murine DED model [546]. Topical COX-2/EP receptor inhibitors reduce the number of CCR7+CD11b+ cells on the ocular surface with inhibition of cellular lymph node homing and suppression of Th17 driven immune responses. Dry eye-induced loss of conjunctival goblet cells was reversed, and corneal erosion was improved by each topical treatment [546].
A number of topical corticosteroid preparations can be used to modulate anterior segment inflammation and multiple studies have shown the clinical value of their short-term use in managing DED. Several RCTs have been published investigating the value of using various corticosteroid formulations in the management of DED (Table 8) [547–557].
Of recent interest is that imaging (rather than clinical evaluations typically associated with dry eye assessment) may also be valuable in establishing the predictive potential for the management of DED with topical corticosteroids [555,558].
While it appears that topical corticosteroids may be valuable in the management of DED, their long-term use is not without risk of complications. These include ocular hypertension, cataracts and opportunistic infections, even after short periods of use [547]. For patients with moderate-to-severe disease that is not controlled with other therapies, repeated short-term pulse therapy of corticosteroids can be an alternative approach. Fifty-three patients with Sjögren syndrome were treated with topical non-preserved 1% methylprednisolone 4 times a day for 2 weeks, and then re-evaluated and tapered off the medication until they demonstrated no corneal fluorescein staining or symptoms [559]. Most patients were in a disease-free state for a relatively long period (57 weeks) after the first pulse therapy, and 11 individuals (21%) experienced a recurrence of either symptoms or signs. After the second pulse therapy, a disease-free period of 72 weeks was observed and only 1.9% of patients had a recurrence. No serious complications (such as IOP elevation or cataract formation) were encountered during the entire follow-up period [559].
The use of topical steroids such as fluorometholone and loteprednol may also be considered, which have a lower likelihood of increasing IOP and inducing cataract formation [560–562]. However, even fluorometholone has been reported to cause cataract after a continuous 4-month application period [563]. A recent retrospective safety study, listing 77 published studies, concluded that topical treatment with loteprednol etabonate has minimal effect on IOP when used in the treatment of a wide range of ocular surface and intraocular inflammatory disorders, including ocular allergy, DED, anterior uveitis, penetrating keratoplasty, endothelial keratoplasty, and postoperative pain and inflammation following ocular surgery [564].
In a prospective, double-masked, multicenter RCT, 0.5% loteprednol therapy two weeks before the initiation of long-term topical 0.05% cyclosporine provided more rapid improvement in Schirmer score, corneal fluorescein staining, lissamine green staining, and symptoms, than topical cyclosporine or artificial tears alone [554]. Loteprednol etabonate induction therapy significantly decreased the incidence of severe stinging and discontinuation of topical cyclosporine [554]. Similarly, treatment with topical 1% methylprednisolone and cyclosporine for an initial three-week period provided faster symptom relief and improvement in ocular signs than topical cyclosporine alone [565].
It has become accepted that preservative use in DED is damaging to the ocular surface [98,566,567], and thus the use of preservative-free topical steroids is growing. In a randomized, parallel-group, case-control study, the efficacy of preservative-free 0.1% HA and 0.1% fluorometholone combined with 0.05% cyclosporine was compared with the efficacy of preserved 0.1% HA and 0.1% fluorometholone combined with 0.05% cyclosporine, in treating DED [118]. The preservative-free eye drops improved subjective symptoms, TBUT, Schirmer score and impression cytology findings more than preserved eye drops [118]. Similarly, a retrospective review of 31 patients treated with preservative-free 0.01% topical dexamethasone showed a significant subjective improvement in symptoms in 84% of the subjects with chronic ocular surface irritation, and/or tearing, refractory to various preserved topical steroids, including 0.2% loteprednol, 0.1% fluorometholone and 1% prednisolone [553]. Further details on this topic are covered in the TFOS DEWS II Iatrogenic Dry Eye Report [102].
A considerable body of basic science and clinical research has investigated the roles of sex steroids (androgens, estrogens and progestins) in the regulation of ocular surface tissues and the adnexa. Clinical studies have also explored the efficacy of these hormones in the treatment of DED. This information is detailed in the TFOS DEWS II Sex, Gender, and Hormones Report [353].
With the exception of cyclosporine, comparatively few clinical trials have been performed using immunomodulating medications in individuals with DED, but demonstration of efficacy within this therapeutic group offers potentially important clues into disease pathogenesis, and may stimulate further research that could lead to commercial development of compounds that may offer demonstrable patient benefit.
The initial TFOS DEWS report noted the importance of ocular surface inflammation not only in the development of, but as a downstream effect and propagator of, DED, and reviewed a range of therapies that function, at least in part, by anti-inflammatory mechanisms of action [1].
Cyclosporine is understood to be an immunomodulatory drug with anti-inflammatory properties, as well as having other actions relevant to managing DED [568–570]. Cyclosporine is a fungal antimetabolite that inhibits IL-2 activation of lymphocytes [570]. It is used systemically as an anti-rejection treatment in patients with organ transplants [571,572], and in autoimmune diseases [573,574], as well as topically in the treatment of allergic, atopic, limbal stem cell dysfunction and autoimmune ocular inflammatory disease [575–578]. Topical cyclosporine was approved by the FDA for the treatment of moderate-to-severe DED in 2003, based on an improvement in tear production measured by the Schirmer test in 15% of patients, compared to 5% of vehicle-treated controls. Treatment with cyclosporine reduces many markers of inflammation [579,580] and also reduces elevated tear osmolarity [63]. Cyclosporine also has anti-apoptotic effects relevant to the known reversal of the normal epithelial cell/leukocyte relationship in DED [581,582], an effect not produced by corticosteroid treatment [583–585]. Additionally, cyclosporine treatment has been reported to result in recovery of reduced goblet cell density in the conjunctiva of subjects with DED [586,587].
A number of Level 1 [588–591] and Level 2 [592,593] studies (Table 9) and several meta-analyses [594–597] (Table 10) have been published that support the efficacy of cyclosporine in the management of DED. However, the outcome measures (both symptoms and signs) and grading scales differ substantially among these studies, which complicates comparisons of the published work. Nonetheless, taken as a body of work, there is strong Level 1 evidence to support the use of topical cyclosporine in the treatment of DED. However, there are a number of exclusions and caveats. It is important to note that cyclosporine A has been reported to lack efficacy in treating DED from surgical procedures, contact lens use and in thyroid orbitopathy and furthermore has demonstrated amelioration of ocular surface damage in only 53% (9/17) of the randomized clinical trials [595].
Quality of life studies have concluded that topical cyclosporine is cost-effective for the treatment of DED as compared to the use of ocular lubricants [598]. A Level 1 study has also reported the additive value of topical cyclosporine therapy in patients fitted with punctal plugs [306]. Fewer studies have differentiated between ADDE patients and those with EDE, but several Level 1 studies [599–602] (Table 11) have reported positive results (again, with varied outcome measures and scales) following treatment with cyclosporine for evaporative DED/MGD.
Treatment of patients with DED using topical cyclosporine needs to be continued for extended periods of time, as evidenced by the rarity of a clinical “cure” (absence of symptoms following drug discontinuation) [603]. The poor water solubility of cyclosporine makes it difficult to formulate into a topical ocular drop. A novel formulation of cyclosporine 0.1% in an unpreserved single-dose cationic emulsion was recently released in Europe [604]. The active drug formulation was superior to vehicle for change in corneal fluorescein staining from baseline and inflammation reduction, as evidenced by human leukocyte antigen D-related (HLA-DR) response, over 6 months, but there was no symptom change over time by OSDI and 29% of subjects still experienced discomfort on instillation, compared with 9% of subjects using vehicle [604].
Tacrolimus, a macrolide produced by Streptomyces tsukubaensis, was discovered in 1984 in Japan while searching for new immunosuppressive and cancer chemotherapeutic agents. Like cyclosporine, it blocks T-lymphocyte activity, but its immunosuppressive potential is higher than that of cyclosporine [605].
In an open-label, prospective study with 14 patients with GVHD with severe DED and intolerance to topical cyclosporine, patients were instructed to instill 0.03% topical tacrolimus once a day for three months [606]. Dry eye symptoms and signs improved significantly with tacrolimus and the authors concluded that topical 0.03% tacrolimus may be a viable alternative for patients with intolerance to topical cyclosporine or in patients where the response to topical cyclosporine is poor. In a prospective, double-masked study of 0.03% topical tacrolimus instilled twice daily in 24 patients with Sjögren syndrome-related dry eye, the average corneal fluorescein staining and rose bengal scores improved statistically after seven days of treatment and continued to improve over 90 days [607]. The Schirmer and TBUT values were unchanged up to 21 days post-treatment, but did show an improvement after 28 days of treatment, relative to baseline.
A variety of non-steroidal anti-inflammatory drugs (NSAIDs) have been used for DED treatment, including 0.1% pranoprofen [608], 0.1% diclofenac [609,610], 0.4% ketorolac [611], and 0.1% indomethacin [610]. The osmoprotective effect of different NSAIDs was evaluated by Sawazaki et al. in a rat model [612]. Diclofenac was able to suppress hyperosmolarity-induced apoptosis and cell growth arrest. In contrast, bromfenac did not exert such a protective action.
Clinical trials have shown that the use of NSAIDs is followed by a reduction in ocular discomfort in patients with DED [613]. However, sporadic case reports of corneal melting in individuals with severe DED have been published [614]. Thus, most published studies with NSAIDS in DED have a duration of no more than 1 month [608,611,613], despite DED being a chronic disease. The effect of NSAID treatment on corneal sensitivity in normal subjects and in patients with DED has been studied. The results of these trials seem to demonstrate that some NSAIDs, diclofenac in particular, have the effect of reducing corneal sensitivity both in normal subjects and in subjects with dry eye [615]. Therefore, it has been suggested that NSAIDs should be used with caution in patients with Sjögren syndrome [610,616].
In a single-masked, randomized, prospective clinical trial on 32 KCS patients, with or without Sjögren syndrome, Avunduk et al. investigated whether anti-inflammatory drops (corticosteroids and NSAIDs) have therapeutic effects [549]. Subjects randomized to receive artificial tears plus topical corticosteroidal drops had significantly lower symptom severity scores, corneal fluorescein staining and rose bengal staining, and HLA-DR positive cells on days 15 and 30 compared with subjects in control groups. The authors concluded that topical corticosteroids, but not topical NSAIDs, had a beneficial effect on symptoms and signs in moderate-to-severe DED [549].
Lubricin (proteoglycan-4) is a lubricating, mucin-like glycoprotein that was first identified in synovial fluid [617]. More recently, lubricin has been discovered on the ocular surface and in the meibomian glands [618]. It is a highly effective friction-reducing boundary lubricant, at both synthetic and tissue surfaces, functions synergistically with HA [619–621] and possesses anti-inflammatory properties [622–624]. Lubricin has been shown to reduce friction and prevent shear stress at the cornea-lid interface, while lubricin deficiency leads to increased shear stress and corneal staining [618]. Full-length recombinant human lubricin has recently been generated and characterized in vitro [625].
Currently, no lubricin-based lubricants are commercially available. A recent two-week, randomized, double-masked, parallel group study in 39 subjects with moderate DED compared a topical formulation of recombinant human lubricin to a 0.18% HA eye drop [626]. Recombinant human lubricin was found to demonstrate significant improvement in both signs and symptoms of DED compared to HA, with significant improvements in a number of clinical variables, including TBUT, corneal fluorescein staining and eyelid and conjunctival redness.
4.2.4.2 Recombinant human nerve growth factor (RH-NGF)
NGF is involved in the regulation of growth, proliferation and survival of neurons and is found naturally in tears [627–629]. NGF has been reported to have trophic effects on the ocular surface, through activation of tropomyosin receptor kinase A (TrkA) and p75 neurotrophin receptor [630]. NGF and TrkA are expressed throughout the ocular surface, including corneal epithelial cells and sensory neurons [631,632].
Topical application of NGF may enhance the production and functional characteristics of the tear film by improving corneal sensitivity, with an improvement of ocular surface signs in dogs with surgically-induced dry eye [633]. In humans, corneal sensitivity, tear production and visual acuity improvement has also been observed after topical administration of murine-derived NGF eye drops (at a concentration of 200 μg/ml every 2 h for 2 days followed by one drop six times daily until the ulcer healed) [634]. A study in rabbits showed that some of these improvements may be due to nerve regeneration. This study showed that topical NGF sped up the recovery of the subbasal nerve plexus after LASIK surgery [635].
Tavilermide (MIM-D3) is a small-molecule NGF peptidomimetic that increases tear and mucin-like fluids and reduces corneal fluorescein staining in a rat model of dry eye [14,636]. In a Phase 2 randomized clinical trial studying the effect of topical MIM-D3 in patients with DED after exposure to a Controlled Adverse Environment chamber to exacerbate dry eye severity, MIM-D3 1% reduced corneal fluorescein staining and conjunctival lissamine green staining after 28 days of treatment when compared to placebo [637]. Similarly, MIM-D3 5% reduced the symptoms of ocular dryness when compared to placebo. In patients with more severe symptoms, both MIM-D3 1% and 5% concentrations showed a significant reduction in symptoms compared to placebo [637]. However, it should be noted that the MIM-D3 clinical trial did not meet its pre-specified primary endpoints with respect to total corneal fluorescein staining and worst symptom score [637].
Mesenchymal stem/stromal cells (MSCs) suppress inflammation in animal models of myocardial infarction, corneal injury and peritonitis [638–640]. It has been proposed that MSCs reduce inflammation through secretion of tumor necrosis factor (TNF)-α-stimulated gene/protein-6 (TSG-6), which has shown therapeutic effects in experimental models of corneal inflammation [641–643]. In a study that investigated the effect of TSG-6 in murine models of dry eye and Sjögren syndrome, topical application of TSG-6 improved tear production, reduced corneal fluorescein staining, and increased goblet cell density when compared to phosphate buffered saline-treated controls [644]. Additionally, TSG-6 reduced the levels of IL-2, interferon-gamma (IFN-γ), IL-1β, and IL-6 in the intraorbital gland. On the ocular surface, TSG-6 significantly reduced the levels of IL-2, IFN-γ, IL-1β, and IL-6 when compared to controls [644]. In a comparative study evaluating the effects of topical administration of TSG-6, cyclosporine and prednisolone in a mouse model of dry eye, TSG-6 showed a similar effect to cyclosporine and prednisolone, resulting in improved tear production and goblet cell density [642]. Additionally, TSG-6 and cyclosporine had a similar effect, reducing corneal fluorescein staining and repressing the levels of IFN-γ and TNF-α on the ocular surface and within the lacrimal gland [642].
Interleukin-1 receptor antagonist (IL-1Ra) is a protein produced mainly by activated monocytes and tissue macrophages, but also epithelial cells. This protein inhibits the pro-inflammatory action of IL-1α and IL-1β by competitively blocking their binding to the IL-1 cell receptor 1 (IL-1R1); when IL1-Ra binds IL-1R1 there is no signalling generated, hence it is an IL-1 antagonizing ligand [645–647]. The IL-1Ra gene is generally upregulated in inflammatory states [646]. Treatment with topical human recombinant IL-1Ra reduces inflammation in animal models of ocular surface inflammation [647–650]. In a murine model of dry eye, topical treatment with IL-1Ra was more effective than CMC in reducing lissamine green staining and increasing tear secretion. Topical IL-1Ra also reduced aberrant acidification of goblet cell mucins and pathological keratinization [651]. In a study that compared the effects of topical IL-1Ra, cyclosporine and methylprednisolone in mice with dry eye, the reduction of corneal fluorescein staining was comparable among the three treatments. However, only IL-1Ra and methylprednisolone reduced the number of central corneal CD11b + cells, corneal lymphatic growth and the corneal expression of corneal IL-1b [544]. In a Phase 2 randomized clinical trial that evaluated the effects of topical IL-1Ra (anakinra; Kineret®) and vehicle three times a day for 12 weeks, treatment with IL-1Ra 2.5% significantly reduced corneal fluorescein staining when compared to baseline values, and significantly reduced symptoms when compared to the vehicle [652]. Additionally, treatment with IL-1Ra induced complete bilateral corneal fluorescein staining clearance in 29% of subjects, compared to 7% in subjects treated with the vehicle.
TNF-α is a cytokine with pro-inflammatory and co-stimulatory effects in multiple cell types; it regulates immune cell trafficking and activation [653,654]. TNF-α expression is elevated in the conjunctiva and tear fluid in animal models and in patients with Sjögren syndrome and other types of DED [655–657]. Some studies have evaluated the effect of systemic treatment with TNF-α blocking agents such as infliximab and etanercept, with conflicting results being reported [658–661]. A further study, which compared topical infliximab and balanced salt solution to treat mice with induced dry eye, showed that mice treated with infliximab had increased tear volume and decreased levels of conjunctival inflammatory cytokines IL-1β, IL-6, IL-17, and IFN-γ, as well as improved goblet cell density [662]. Researchers have also shown that both TNF-α blockers HL036 and etanercept decreased inflammation in the lacrimal gland and cornea of mice with experimentally-induced dry eye by suppressing IFN-γ, IL-21, and IL-6 [663].
Th17 cells have been implicated in the pathogenesis of numerous autoimmune diseases. An increased expression of Th17-associated cytokine IL-17 has been demonstrated to promote disruption of the corneal epithelial barrier, thus playing a role in the pathogenesis of DED [664–666]. In an in vivo model of dry eye, treatment with IL-17 antibody significantly reduced corneal fluorescein staining in mice [665]. Another study showed that antibody neutralization of IL-17 in mice with experimental dry eye ameliorates corneal epithelial barrier dysfunction (reducing fluorescein permeability) and expression of MMP-3 and MMP-9 [666]. Additionally, treatment with anti-IL-17 antibody has been shown to significantly reduce lymphangiogenesis in mice with dry eye, which may aid in reduction of DED-related immunity [667].
In summary, biologic molecules hold a promising future in the treatment of DED. However, although many biologics have been thoroughly investigated in animal models, human studies remain scarce and well-designed human trials are required to further assess their therapeutic role.
Substance P, calcitonin gene-related peptide (CGRP), neuropeptide Y (NPY) and vasoactive intestinal peptide (VIP) have been evaluated in a variety of lab-based studies and clinical studies on normal eyes and in DED. The decreased tear levels of NPY and CGRP in DED are related to impaired lacrimal function [629]. These findings suggest that NPY and CGRP could become useful biomarkers and have therapeutic activity in dry eye [629,668].
The effect of VIP has been tested on immortalized human meibomian gland epithelial cells [669]. The cells transcribe and translate VIP and mACh receptors; VIP activates the adenylyl cyclase pathway; VIP increases intracellular [Ca2+] in meibomian gland cells; and VIP stimulates meibomian gland cell proliferation when combined with forskolin.
Most of the studies investigating neuropeptides to date have been performed in moderate and severe neurotrophic keratitis with concomitant DED, but not directly in individuals with DED [670].
The range of mechanisms of action of the medications discussed in this section, that have at least some demonstrable efficacy in the treatment of patients with DED, gives some insight into the complex pathophysiology of this disease. Clearly, further research is warranted.
One strategy to inhibit or decrease T cell mediated inflammation in DED is to prevent T cells from interacting with other immunologically active cellular elements. Integrins are heterodimeric cell surface receptors, ubiquitous in a variety of cellular and physiologic processes, including cell adhesion, migration and activation, steps crucial for T cell activity and survival [671]. Of the 24 known integrin heterodimers, the β2 subfamily of integrins is found only on lymphocytes [671]. Lymphocyte function-associated antigen-1 (LFA-1) is a member of this integrin family. The primary ligand for LFA-1 is the intercellular adhesion molecule 1 (ICAM-1), expressed on a variety of cells, including endothelial and epithelial cells and antigen presenting cells [672]. Binding between LFA-1 and ICAM-1 has been described as the “immunologic synapse” and a critical step in the pathway toward T cell activation [673].
Lifitegrast is a small molecule integrin antagonist, engineered to mimic ICAM-1's binding domain to LFA-1 and believed to act as a competitive antagonist to block binding between LFA-1 and ICAM-1, resulting in inhibition of T cell migration into target tissues, reduction of cytokine release, and reduction of further T cell recruitment [674–676].
Lifitegrast 5% ophthalmic solution has been studied as a topical treatment for DED and five clinical trials have been published to-date. In a Phase 2 clinical trial on 230 patients [677], a significant response was observed for the pre-specified secondary endpoints of mean change from baseline to day 84 in inferior corneal staining and for a vision-related function subscale, but not for the primary efficacy endpoint of mean inferior corneal staining. In a Phase 3 clinical study (OPUS-1), involving 588 subjects with DED [678], a significant response was reported in the primary efficacy variable of mean change from baseline to day 84 in inferior corneal staining as well as other secondary efficacy endpoints (total corneal staining and conjunctival lissamine green staining). However, the study did not meet the co-primary endpoint for symptoms (the vision-related function subscale of OSDI), though significant improvement was reported for treated subjects in several secondary efficacy symptom endpoints. A second Phase 3 clinical study, OPUS-2, reported results from 718 participants treated with lifitegrast 5% or placebo over 84 days [679]. In this trial, significant improvement was reported in the primary efficacy endpoint (change from baseline to day 84 in Eye Dryness Score; visual analog scale) as well as the secondary symptom endpoint of ocular discomfort. However, improvement was not observed in lifitegrast-treated subjects in the co-primary endpoint of mean change from baseline to day 84 in inferior corneal staining, in contrast to the results from OPUS-1. The SONATA long-term safety study reported on 331 patients treated with lifitegrast twice daily or placebo for 350 days [680]. Lifitegrast appeared safe and well tolerated with no serious ocular adverse events reported and a safety profile that was similar to that of the previously published studies.
Taken together, these Level 1 studies demonstrated the efficacy of lifitegrast, and the FDA approved Xiidra™ (lifitegrast 5% ophthalmic solution Shire, Lexington, MA, USA) in a single dose unit format, in July 2016, for the treatment of both signs and symptoms of DED.
Tetracycline and its analogues (minocycline, doxycycline) are broad-spectrum antibiotics that inhibit protein synthesis by inhibiting the binding of aminoacyl-tRNA to the mRNA-ribosome complex. It is hypothesized that a decrease in bacteria-producing lipolytic exoenzymes [681,682], and inhibition of lipase production [683], with resultant decrease in meibomian lipid breakdown products, may contribute to improvement in clinical parameters in MGD and anterior blepharitis associated with DED. These agents also have anti-inflammatory properties. They decrease the activity of collagenase, phospholipase A2, and several MMPs, and decrease the production of inflammatory mediators such as IL-1 and TNF-α in a wide range of tissues, including the corneal epithelium [541,542,684–686]. In experimental murine models of dry eye, topically applied doxycycline was found to preserve corneal epithelial smoothness and barrier function [541,542], and to alleviate ocular surface inflammation [687]. Similarly, minocycline decreases the production of diglycerides and free fatty acids in meibomian secretions [681]. However, evidence exists to suggest that doxycycline, tetracycline and minocycline do not duplicate the ability of azithromycin to stimulate differentiation and lipid accumulation in human meibomian gland epithelial cells [688].
Tetracycline and its analogues are often used to treat disorders that are associated with DED such as acne rosacea, MGD and blepharitis. Doxycycline and minocycline achieve a higher concentration in tissue and have a lower renal clearance, longer half-life and higher level of binding to serum proteins than tetracycline and oxytetracycline [689], and are often prescribed in cases of ocular inflammatory diseases because of these properties.
Rosacea, including its ocular manifestations, is an inflammatory disorder that occurs mainly in adults, with peak severity in the third and fourth decades. Evidence exists to suggest that it is strongly correlated with MGD [690] and that Demodex infestation may be associated with its development [691–694]. Strong evidence exists that topical azelaic acid, ivermectin, brimonidine, doxycycline and isotretinoin, and oral tetracyclines (doxycycline and minocycline) are effective treatments for rosacea [695,696]. However, strong evidence also exists to show that isotretinoin destroys human meibomian glands and induces keratinization of the meibomian gland ducts [477,697], and thus its topical use for treatment of the ocular surface may not be advisable.
Tetracycline and its analogues have been shown to reduce subjective symptoms and hyperemia associated with ocular rosacea in small clinical case series [698,699], with a single daily dose of doxycycline as low as 40 mg proving to be effective [700,701]. A prospective, randomized, double-masked, placebo-controlled, partial crossover trial, compared the ability of oxytetracycline to provide symptomatic relief of blepharitis, in 43 patients with and without rosacea [702]. Only 25% of the patients with blepharitis without rosacea responded to the antibiotic, whereas 50% responded when both diseases were present. A comparative prospective interventional study consisting of 44 subjects showed that elevated tear levels of MMP-8 on the ocular surface of individuals with rosacea was found to be reduced significantly after 4- and 8-week treatment with oral doxycycline [703]. A review suggested that additional Level 1 studies are necessary to further assess the efficacy of tetracyclines in the management of ocular rosacea [696].
Chronic blepharitis is typically characterized by inflammation of the eyelids and there are many sub-types of this condition [381]. Tetracyclines are used to treat chronic blepharitis due to their antimicrobial and anti-inflammatory effects and several studies have described the beneficial effects of minocycline and doxycycline [681,683,704]. However, to-date there are no randomized, controlled, double-masked RCTs that demonstrate the efficacy of antibiotics over lid hygiene or other treatments [705,706].
The effects of tetracyclines in patients with MGD have been reported in a case report [707]. A randomized, unmasked prospective controlled study compared different doxycycline doses in 150 patients who had chronic MGD and who did not respond to lid hygiene and topical therapy for more than 2 months [708]. Subjects were randomized into three groups: a high dose group (doxycycline, 200 mg, twice a day), a low dose group (doxycycline, 20 mg, twice a day) and a control group (placebo). After one month, both the high- and low-dose doxycycline groups demonstrated statistically significant improvements in TBUT and symptoms.
A randomized, double-masked, placebo-controlled cross-over study was conducted to investigate the efficacy of low dose doxycycline at 20 mg twice daily to treat clinical symptoms of Sjögren syndrome [709]. Only 5 of the 16 subjects on doxycycline reported significant improvement in their symptoms. Another prospective, randomized unmasked clinical trial consisting of 60 subjects with moderate-to-severe MGD showed that minocycline at the daily dose of 50 mg significantly improved clinical signs of MGD, including TBUT, conjunctival and corneal staining, eyelid appearance and meibum quality, than a control group treated with ocular lubricants [710]. Ocular surface inflammatory mediators including IL-6, IL-1β, IL-17α, TNF-α, and IL-12p70 were found to be significantly reduced after two months of treatment [710].
The optimal dosing schedule of tetracyclines for treating DED has not been established, with a variety of dosing regimens having been proposed. These include 50 or 100 mg doxycycline once a day [711], 200 mg twice daily for 1 month followed by 200 mg daily, or an initial dose of 50 mg a day for the first 2 weeks followed by 100 mg a day for a period of 2.5 months, in an intermittent fashion [681–683,707]. Others have proposed the use of a low dose of doxycycline (20 mg) on a long-term basis [708].
In addition to the known side effects of tetracyclines, which include gastrointestinal symptoms and photosensitivity, safety issues associated with long-term antibiotic therapy have been raised. To minimize risks, a recent study suggested that a three-month course of 100 mg of minocycline might be sufficient to bring significant meibomianitis under control, as continued control was maintained for at least three months after cessation of therapy [707]. Doxycycline (40 mg daily) is the only tetracycline approved by the FDA for up to 16 weeks in the treatment of rosacea. Long-term doxycycline treatment at this level does not exert antibiotic selection pressure on the microbiota, preventing the development of antibiotic resistance [712,713]. These recommendations may be tempered by reports that, in women, the risk of developing breast cancer and breast cancer morbidity increases cumulatively with duration of antibiotic use, including tetracyclines [714,715], although another study did not substantiate these findings [716]. Additional studies are needed to determine if there are risks with long-term tetracycline use.
Some reports exist concerning the positive impact of systemic azithromycin in the treatment of MGD, especially in people suffering from intolerance to other systemic antibiotics [717–720]. A recent laboratory-based study compared the effect of azithromycin, doxycycline, minocycline or tetracycline for 5 days on immortalized human meibomian gland epithelial cells [688]. Azithromycin, but not the other antibiotics, significantly increased the cellular accumulation of cholesterol, cholesterol esters, phospholipids, and lysosomes. The authors concluded that the stimulatory effects of azithromycin on human meibomian gland epithelial cell function are unique and not duplicated by the other antibiotics evaluated [688].
Azithromycin can be a valuable option when MGD occurs in association with rosacea [721–723], and it is believed that its anti-inflammatory properties may help control bacterial flora and lid inflammation [706,724–726]. The most common side effects of oral azithromycin are diarrhoea, nausea and vomiting.
The ideal dosage of systemic azithromycin is still controversial and there is no universal agreement. Previous studies have shown efficacy with a daily oral dose of 250 mg or 500 mg for the treatment of rosacea [721,723,727]. A pulse treatment with oral azithromycin for pustular acne has been proposed [728,729], and the same concept appears to be successful for MGD management, using 500 mg per day for 3 days in 3 cycles with 7-day intervals [720]. Further double-masked RCTs must be performed to clarify long-term efficacy and ideal dosing.
Table 12 summarizes several clinical studies investigating the use of both oral and topical azithromycin in the management of DED [720,730–735]. Where available, topical 1% azithromycin is well tolerated and appears to be effective in the management of MGD and evaporative DED, although the low number of well-designed studies still makes this a somewhat controversial therapy. In a recent large scale study by Hosseini and colleagues evaluating 907 subjects with blepharitis, a combination of topical azithromycin–dexamethasone used for 14 days twice daily was safe and well tolerated [735]. This combination drop achieved complete clinical resolution in a greater percentage of patients (8.2%) than 1% azithromycin (5.2%), 0.1% dexamethasone (5.7%), or vehicle (4.7%).
Whether there is benefit in combining systemic and topical azithromycin to improve the treatment of evaporative DED, especially in the management of refractory or severe cases, requires further study.
To date, two studies have compared the efficacy of doxycycline and azithromycin for the management of MGD [717,736]. A five-day oral azithromycin regimen was compared to one month of doxycycline (200 mg) in one study (Level 2 evidence) [717]. Although both treatments significantly improved clinical scores and symptoms, azithromycin appeared be more effective in improving clinical signs. In the second Level 2 study, both topical 1% azithromycin for four weeks and twice daily 100 mg oral doxycycline for two months significantly decreased the clinical signs of MGD. Oral doxycycline treatment was slightly less effective in improving foreign body sensation and the signs of plugging and secretion than topical azithromycin [736].
Of note, is a recent report that evaluated the role of oral antibiotics for meibomian gland-related OSD [737]. This review concluded that there is no Level 1 evidence, and only scant evidence overall, to support the use of oral antibiotics in the management of meibomian gland-related OSD.
Tarsorrhaphy refers to a temporary or permanent surgical procedure in which the eyelids are partially or totally closed using sutures. In addition to temporary closure with sutures, a temporary tarsorrhaphy can also be achieved with adhesive tape, glue or levator paralysis by botulinum toxin injection [738]. Any form of tarsorrhaphy decreases ocular surface exposure, reduces evaporation of the tear film and ultimately results in reduced ocular surface desiccation and drying. The procedure is mainly performed in cases of persistent epithelial defects and reserved for severe dry eye that is refractory to medical treatments and punctal occlusion [499]. Possibly due to the fact that it is normally reserved as the last step when all other treatments have failed, only 20% of patients reported being unhappy with the aesthetic effects [739].
To-date, there are no studies comparing the efficacy of tarsorrhaphy to other treatment modalities in DED.
Conjunctivochalasis is characterized by loose, redundant, non-edematous inferior bulbar conjunctiva that is located between the globe and the eyelid. This is an age-related ocular disorder, which is often overlooked and negatively impacts quality of life [740]. Conjunctivochalasis is a common finding in dry eye, with a reported prevalence of 54% in individuals with DED [741], and another report suggesting that its presence has a positive predictive value of 93% in the diagnosis of DED [742]. The severity of conjunctivochalasis can be graded by recording the lid-parallel conjunctival folds (LIPCOF) score, with a higher grading positively correlating with more severe dry eye symptoms [743]. The mechanism linking conjunctivochalasis with dry eye symptoms could relate to its impact on the lower TMH [744,745]. Epiphora is also a symptom of conjunctivochalasis, especially when it is located medially, and can be alleviated by correction of conjunctivochalasis [746,747].
In severe cases of conjunctivochalasis that do not respond to ocular lubricants, topical cyclosporine or punctal occlusion, resection of the excessive conjunctival tissue may be considered [748]. Several approaches to reduce the excessive conjunctival folds have been reported, including electrocoagulation or thermal cauterization [749,750], simple fixation to the sclera [751], and Argon laser conjunctivoplasty [752]. In all studies (Level 3 evidence), some level of improvement in symptoms has been reported in over 75% of patients.
Essential blepharospasm (EB) is a focal cranial dystonia involving the eyelid and forehead muscles. It has been reported that 40–60% of EB patients have dry eye symptoms and decreased Schirmer scores [753–756]. Additionally, pro-inflammatory cytokine levels in the tear fluid are also increased in dry eye patients with EB, compared to those with only DED [757].
Botulinum toxin A injection for the management of EB causes a temporary pharmacologic denervation of the orbicularis oculi muscle. Several case-control studies (Level 2 evidence) report amelioration of dry eye symptoms and an increase in TMH, TBUT and tear clearance time after botulinum toxin A injection [757–759]. However, these effects last for only 3 months [760]. In contrast, tear production can possibly be impaired by botulinum toxin A injections that occur too close to the lacrimal gland [753,761,762].
Dermatochalasis is a term used to describe the presence of loose and redundant eyelid skin and is a common sign of aging. Based on Level 2 and 3 evidence, 46–51% of patients with dermatochalasis have dry eye complaints and 55–86% of patients achieve subjective improvement in symptoms after upper eyelid blepharoplasty [763,764]. However, objective parameters have not been shown to change significantly after blepharoplasty [764], and the reported improvements may be purely psychological.
Dry eye disease can be a risk factor for blepharoptosis, as it causes increased friction between the upper lid and the ocular surface, which may contribute to disinsertion or thinning of the levator aponeurosis. A prospective case-control study (Level 2 evidence) showed that a low Schirmer score occurs more often in patients with acquired aponeurogenic ptosis than in controls [765].
Despite surgical correction of ptosis, tear quality can continue to deteriorate. In an interventional case series, Schirmer scores and TBUT revealed a decrease in tear quantity and quality after surgery [766]. Tear volume may also decrease after ptosis surgery [767,768].
Lower lid laxity and ectropion are common occurrences with increasing age and are most commonly treated with transcutaneous lower lid blepharoplasty. However, even after apparently successful surgery, patients often complain of dryness, epiphora and chemosis postoperatively [769–771].
Dry eye disease is one of the most common complications after any kind of eyelid surgery [102], with the exception of tarsorrhaphy [772]. Common causes of postoperative dry eye include chemosis, increased exposure of the ocular surface, lagophthalmos, lower eyelid malposition, or diminished blink reflex from surgical anesthesia or oedema [102,483]. These are described in more detail in the TFOS DEWS II Iatrogenic Dry Eye and Pathophysiology Reports.
Individuals with conjunctival disorders such as pterygium, pingueculae, Stevens-Johnson syndrome, and mucous membrane pemphigoid often develop DED. Advanced pterygium results in an uneven distribution and focal evaporation of tears over the ocular surface, aggravating dry eye symptoms. Dry eye patients with severe ocular surface inflammation and cicatrization could benefit from surgical treatment with conjunctival reconstruction, as well as removal of the inflamed tissues and activated fibroblasts [773–775]. However, in patients with mucous membrane pemphigoid, any ocular surface and eyelid surgery should be performed after the disease is adequately controlled by systemic immunosuppression to avoid exacerbation of the disease. Conjunctival or limbal autograft reduces pterygium recurrence compared to bare sclera excision and amniotic membrane transplantation, and has become a standard treatment [776]. Concurrent application of mitomycin C application further reduces the risk of recurrence, however this is associated with potentially serious complications such as scleral thinning, ulceration, and delayed conjunctival epithelialization [777].
Severe DED can lead to persistent epithelial defects, corneal ulceration and corneal scarring. Amniotic membrane grafts could be considered for persistent epithelial defects in cases of ocular cicatricial pemphigoid, Stevens-Johnson syndrome and other severe OSD [499,775,778–782]. These membranes contain a wide variety of neuropeptides and neurotransmitters, including acetylcholine and catecholamine [783–787].
A particular form of amniotic membrane transplant is the PROKERA® and thinner PROKERA® SLIM (Bio-TissueDoral, FL, USA). These devices contain human amniotic membrane processed with a form of cryopreservation that retains the tissue's biological activity. The membrane is contained within a thermoplastic ring that permits the device to be inserted in a similar manner to a scleral lens and holds the tissue firmly in place. The grafts typically dissolve in approximately one week and the conformer ring can then be removed [788]. To date, only a few case studies have been published on its use [782,789,790]. One study did show sustained symptom improvement for four months in dry eye subjects who wore the PROKERA® SLIM for approximately five days on average [782]. The authors also reported reduced corneal and conjunctival staining and improved visual acuity.
In severe DED, individuals with Schirmer scores of ≤ 1 mm may require the application of lubricating drops every few minutes, which seriously disrupts daytime activities and results in a marked reduction in quality of life. In these cases, mechanical devices that deliver lubricating drops from a reservoir through a catheter have been used to continuously lubricate the ocular surface. A rabbit study showed that a microinfusion pump, originally developed for insulin treatment in diabetics, was able to deliver a dose of artificial tears that was similar to that found in normal eyes [791]. In addition, eyes treated with corticosteroid delivered by this pump recovered faster than those treated with topical corticosteroid.
In a prospective, non-randomized trial of 21 subjects with a Schirmer score of ≤ 1 mm, a 60 ml reservoir was implanted under the subcutaneous tissues of the anterior abdominal wall and connected to a silicone catheter that ascended subcutaneously along the chest, neck and temple to the upper conjunctival fornix [792,793]. All subjects reported an improvement in symptoms and exhibited prolonged TBUT with a reduction in corneal staining and conjunctival hyperemia. Infections of the reservoir or the catheter, although not reported in this study, can occur, and may require explantation of the device.
While rare, it is clear that mechanical dacryoreservoirs may be a valuable option in cases of very severe aqueous tear deficiency, where all other less invasive measures have failed to achieve sufficient subjective relief.
The aim of salivary gland transplantation is to provide some functioning exocrine tissue to a severely dry eye. Possible indications can include primary (congenital) alacrimia or severe aqueous deficiency secondary to cicatricial conjunctivitis (due to mucous membrane pemphigoid, Stevens-Johnson syndrome, chemical burns), surgical damage or radioablation of lacrimal tissue (such as that found in neoplastic disease of the head). Having a functional salivary gland will, in addition to being a constant source of lubrication, also provide epitheliotrophic factors that are also present and functionally relevant in the tears [794].
The three major salivary glands, the parotid, submandibular and sublingual gland, have all been used to lubricate the ocular surface, although the approach of transplanting a sublingual gland to the subconjunctival space has failed to succeed, due to ischemia of the grafted tissue [795]. For the parotid gland and the submandibular gland the surgical approaches are entirely different and both require the expertise of an experienced oral surgeon.
In this procedure, the secretory duct of the parotid gland is moved from its original premolar position in the mouth to the lower conjunctival fornix [796]. Since the innervation of the gland is maintained, a gustatory reflex epiphora of a purely serous secretion results. Evidence for its success is limited to retrospective case reports or series without quantitative follow-up data. Complications include blepharitis and keratitis from excessive secretion, for which measures such as systemic anticholinergics or parasympathetic denervation of the gland were found to be either impracticable or ineffective and this technique seems to have been abandoned [797].
A free partial or total submandibular gland with a vascular pedicle and the secretory duct are transferred to the temple. A microvascular anastomosis with facial vessels is created and the duct sutured into the conjunctival fornix [798,799]. While the procedure requires several hours of general anesthesia, it offers some major advantages over other procedures using salivary gland tissue, including (i) an established blood supply to ensure the glands' viability, (ii) a secretion capable of replacing the mucous and serous component of the tear film, (iii) absence of reflex salivation due to intraoperative sympathetic denervation of the graft and (iv) a maintained baseline secretion due to surviving parasympathetic intraglandular ganglion cells [800].
In rats and rabbits, transplanted submanidibular glands remained viable and active for at least six months post transplantation [801,802]. Several groups have published clinical results in subjects with severe aqueous deficiency [798,799,803–807]. Despite the potential for microvascular complications, a reported 66–100% remained viable for at least five years, according to clinical ophthalmological examination or scintigraphy [808]. Allogeneic grafts require long-term immunosuppression [809]. Most reports come from maxillofacial or ear, nose and throat surgeons and often have only limited data on specific ocular surface findings. The most systematic evaluation to-date is a prospective, controlled case series with a follow-up of more than 40 months [805,807]. The results showed a substantial improvement in Schirmer score, TBUT, use of tear substitutes and symptoms compared to controls (fellow eyes without a viable submanidibular gland graft) from three months through to the end of follow-up. Neither visual acuity (probably due to pre-existing corneal scarring and other comorbidities) nor conjunctival inflammation or squamous metaplasia improved [807].
When comparing total versus partial submanidibular glands transplantation, Qin and coworkers reported severe epiphora in 19 out of 22 patients with a total submanidibular gland graft, versus 6 out of 20 eyes with a partial transplant [799]. Secretion from the gland was stimulated by heat or physical activity and could be blocked by anticholinergics [799,805,810,811]. Hypersecretion can also be controlled surgically by reducing the size of the gland or by partial ligation of the duct [805,812].
While the resulting lubrication contains many proteins and other components abundant in tears, it is very hypo-osmolar compared to tears and this hypo-osmolarity can induce microcystic epithelial oedema in cases with oversecreting transplants [190,794,807,813]. As a consequence, 100% of five corneal transplants performed following submanidibular gland transplantation failed, due to rejection, infection, calcification or epiphora-associated epithelial oedema, with subsequent corneal perforation [807].
In summary, the submanidibular gland is the only major salivary gland that is currently being used to supply lubrication to the eye by means of transplantation. It is only indicated in patients with absolute aqueous tear deficiency with persistent severe discomfort and when all other means have failed. These patients benefit from substantial relief of severe symptoms and some signs of dry eye, but the procedure does not enable successful visual rehabilitation.
Oral and nasal mucosa can be used to reconstruct the fornices and to provide mucin to the ocular surface, but this procedure fails to provide sufficient lubrication to sustain a healthy corneal graft [814,815]. Labial mucosa (which lines the lips) has been used as a complex graft to the conjunctival fornix in severe dry eyes, with excellent success in terms of graft viability [795,797]. The secretion of the minor salivary glands is predominantly mucinous, with the buccal salivary glands showing the highest flow rate [816]. Transplantation resulted in an increase in Schirmer test score and TBUT and also provided symptomatic relief [817].
Marinho reported results of 14 and Sant’ Anna, of 19 patients with severe DED secondary to Stevens-Johnson syndrome who had labial salivary gland transplantation [817,818]. Up to 14 months postoperatively, tear volume was improved in over 70% of patients. Corneal transparency and visual acuity improved in 72% and symptoms decreased in 54% and 100% respectively. Potential complications include temporal labial hypoesthesia or graft necrosis, the feeling of “watery” eyes or bulkiness and laxity of the eyelids leading to entropion, as well as donor site morbidity.
There is growing evidence that diet and nutritional supplementation play a role in DED. The contributions of general hydration status, and other interventions, such as lactoferrin and anti-oxidant supplementation, are also worthy of consideration.
Whole-body hydration status has been proposed to have a potential role in DED control. Tear osmolarity levels in healthy adults increase as a result of modest whole-body dehydration (2–3% body mass loss) during exercise [819,820], an effect that is modifiable with fluid intake [819]. Observational data suggest that whole-body hydration status may also directly influence the clinical expression of DED. In a cross-sectional study of 111 participants aged at least 60 years, individuals classified as having DED were found to have higher plasma osmolality, indicating sub-optimal hydration, than individuals without DED [821]. Whether improving whole body hydration with fluid intervention confers a therapeutic benefit in people with DED requires further study. Specifically, there remains the need for controlled intervention trials to assess the efficacy and safety of optimizing hydration status as a non-drug therapy for DED.
Essential fatty acids (EFAs) are termed ‘essential’ as they are necessary for healthy metabolic processes to occur [822]. Humans are unable to form EFAs in vivo and must ingest them from dietary sources. Two key EFAs are the 18-carbon omega-3 (ω-3) and omega-6 (ω-6) fatty acids. The ω-3 EFAs exist as both short (alpha-linolenic acid, ALA) and long-chain (eicosapentaenoic acid, EPA and docosahexaenoic acid, DHA) sub-types. Both subtypes can be consumed from food, with long-chain forms also capable of being produced from short-chain forms within the body, through the desaturation/elongation of short-chain EFAs. Common food sources for ALA include flaxseeds, walnuts, chia seeds and soybean oil. The long-chain ω-3 polyunsaturated fatty acids (PUFAs), EPA and DHA, are present in high concentrations in oily fish (such as tuna, salmon, trout, sardines and mackerel) and to a lesser extent in shellfish (such as prawns, oysters and mussels). The ω-6 EFAs are commonly derived from vegetable oils, such as safflower oil and corn oil, in the form of linolenic acid (LA), which, once ingested, is desaturated and elongated to gamma-linoleic acid (GLA) and arachidonic acid (AA) [823].
Within the body, ω-3 and ω-6 EFAs compete for the enzymes that regulate their metabolism, to produce eicosanoids that modulate systemic inflammation. Eicosanoids derived from the ω-6, AA-dependent pathway, including prostaglandin-E2 (PGE2), thromboxane-A2 and leukotriene-B4, are pro-inflammatory. While most ω-6 eicosanoids promote inflammation [824], metabolism of GLA can result in the production of prostaglandin-E1 (PGE1) and thromboxane-A1, which are anti-inflammatory mediators [824]. The potential effect(s) of ω-6 EFAs on inflammation is therefore complex. Long-chain ω-3 EFAs bias prostaglandin metabolism towards the production of anti-inflammatory eicosanoids, including resolvins and protectins, which are essential for limiting and resolving inflammation [825]. As such, the relative ratio of consumed ω-3 to ω-6 EFAs influences the overall inflammatory status of the body [824].
In modern times, the balance of ω-3 to ω-6 essential fatty acids (EFA) dietary intake has shifted, thereby altering the balance of inflammatory cytokines [826]. In current Western diets, the ratio of ω-6:ω-3 intake is typically 15:1, whereas an ideal ratio is generally considered to be 4:1 [827]. As a result, there has been scientific interest in understanding whether increasing systemic ω-3 EFA levels through nutritional intervention, to lower the ω-6:ω-3 ratio, can yield systemic anti-inflammatory effects that are beneficial for conditions with an inflammatory overlay, including DED.
Omega-3 EFAs are recognized to have a broad range of systemic anti-inflammatory effects, including inhibiting the production of several key pro-inflammatory cytokines (such as IL-1, IL-2 and TNF-α) [828–830] and preventing T-lymphocyte proliferation [831,832], processes that have been implicated in the pathogenesis of DED.
Several laboratory studies have shown that fatty acid enrichment can impart lacrimal gland changes and alter the ocular surface response to pharmacologic-induced models of DED [833–838]. Two recent laboratory-based studies have evaluated the impact of EFAs on the function of human meibomian gland epithelial cells [833,834]. The study by Liu et al. showed that EFAs influence the quality and quantity of intracellular lipids, resulting in a 2.4- to 3.7-fold increase in the cellular content of triglycerides after ω-3 and ω-6 treatment, respectively. In rats, dietary supplementation with ω-3 (EPA + DHA) for three months was associated with their incorporation into lacrimal gland tissues [835]. Two-month dietary enrichment with combined ω-3 (EPA + DHA) and ω-6 (GLA) PUFAs, reduced corneal keratitis, minimized the overexpression of conjunctival major histocompatibility complex (MHC) II and inhibited upregulation of prostaglandin (PG) E1 and PGE2 in the lacrimal gland, after 28 days of scopolamine intervention [836]. In murine DED models, topical formulations of ω-3 EFAs have been shown to reduce levels of corneal fluorescein staining [837,838], and decrease both CD11b (+) cell numbers and conjunctival expression of IL-1α and TNF-α [837]. Topical ω-3 EFAs, with and without added 0.1% HA, have also been found to improve corneal irregularity and reduce epithelial barrier disruption [838].
Experimental evidence supports the therapeutic potential of a class of endogenous lipid-derived immunomodulators, resolvins, derived from EPA (resolvin E1) and DHA (resolvin D1), as an anti-inflammatory treatment for DED [14,839,840]. Resolvins E1 and D1 promote the resolution of inflammation in cultured conjunctival goblet cells by reducing cysteinyl leukotrienes [839,840]. In murine DED models, resolvin E1 has been reported to increase tear production, improve corneal regularity and decrease macrophage infiltration [841], and to reduce corneal epithelial barrier disruption and attenuate conjunctival goblet cell loss [842]. Topical application of a prodrug of resolvin E1, RX-10045 (0.1%), which is rapidly hydrolyzed to its active form in biological matrices, can reduce corneal stromal haze after rabbit corneal injury [843]. In a recent clinical study RX-10045 failed to meet a primary endpoint related to corneal staining [329]. While investigations involving resolvin D1 are less prevalent, it should be noted that these agents have a role in corneal health. For example, a derivative of DHA, NPD1, is important in nerve regeneration and corneal sensitivity [844,845].
The Women's Health Study, involving over 32,000 women, described an association between a low dietary intake of ω-3 EFAs and DED in women [846]. This study reported a 30% reduction in the risk of DED with each additional gram of ω-3 EFAs consumed per day. A higher ratio of dietary ω-6:ω-3s was also associated with an elevated risk of DED (for ≥15:1 versus <4:1, odds ratio: 2.51; 95% CI: 1.13, 5.58, p = 0.01). Furthermore, it has been recently shown that the ratio of ω-6:ω-3 tear lipids is elevated in people with DED and that this occurs in proportion to the degree of tear film dysfunction and corneal staining [847]. The level of dietary ω-3 EFA intake is also associated with differences in the polar lipid pattern of meibomian gland secretions in women with Sjögren syndrome [848].
Clinical trials have been undertaken to assess the potential benefit of oral ω-3 and ω-6 EFA supplementation, both alone and in combination, for treating DED. Most of these intervention trials have been performed at single sites and with relatively small participant numbers (sample size <70). The clinical trials have had varying degrees of masking, of both participants and outcome assessors, with few being double-masked.
All of the clinical trials evaluating ω-3 EFAs alone (Table 13) [849–859] have been undertaken for three months or less, with the exception of one pilot study that investigated the efficacy of short-chain ω-3 EFAs (ALA) for treating MGD and blepharitis over 12 months [849]. The ω-3 EFA interventions have varied both in terms of subtype (short- and/or long-chain formulations) and dose. To date, only one study has evaluated the relative efficacy of different forms of long-chain ω-3 EFAs for treating DED, comparing krill oil, in primarily phospholipid form, to fish oil, in triacylglyceride form [858]. This randomized, placebo-controlled clinical trial suggested that ω-3 EFAs in phospholipid form (krill oil) might confer additional therapeutic benefit in DED, with further clinical investigations needed to assess this potential. A variety of outcome measures have been examined, primarily involving quantifying changes to patient symptomatology and objective clinical measures relating to tear stability and/or production. More recently, beneficial effects with oral ω-3 EFA supplements in DED have also been demonstrated, with the specification of tear osmolarity as a primary outcome measure [858,859]. A recent pilot study has further demonstrated central corneal neuroprotective effects with a three-month supplementation of a moderate dose of ω-3s (1000 mg/day EPA + 500 mg/day DHA) in DED [860]. Attempting to summarize the best available evidence, a meta-analysis concluded that ω-3 EFA supplementation improves TBUT and Schirmer scores in individuals with DED, without significantly altering OSDI scores [861].
Although many patients self-medicate with ω-3 EFA supplements on the premise of their well-publicized health benefits, use of these supplements requires some precautions. There are several important systemic contra-indications, including liver disease, atrial fibrillation and bleeding disorders; in these cases, medical advice should be sought prior to commencing supplementation. There may be potential risks to health with high-dose ω-3 EFA intake (>2000 mg/day combined EPA + DHA), in terms of a heightened risk of bleeding [862], and people with hematological disorders should seek medical advice before consuming ω-3 EFA supplements [863]. The possibility that males with high serum concentrations of long-chain ω-3 PUFAs have a heightened risk of prostate cancer has also been raised [864], but remains contentious [865,866]. Both the FDA and the National Health and Medical Research Council (NHMRC) in Australia recommend an upper daily limit for omega-3 fatty acid consumption of 3 g (3000 mg); this includes omega-3 fatty acids derived both from food and supplements. It is important to note that this dosage relates to the amount of omega-3 fatty acid content, rather than the size of the supplement capsule per se. For example, many 1 g (1000 mg) fish oil capsules contain 180 mg EPA + 120 mg DHA; thus only about 30% of the content of the fish oil supplement capsule will be long-chain omega-3 fatty acids.
Interventional clinical trials that have evaluated ω-6 EFA formulations for treating DED have been performed at single-sites, ranging in duration from three weeks to six months, and with considerable variations in daily dose (Table 14) [867–871]. Most studies targeted study populations with Sjögren syndrome, with variable outcomes reported in relation to changes in dry eye symptoms, ocular inflammatory markers and other clinical signs (such as ocular surface staining, TBUT, Schirmer score).
Clinical trials that investigated supplementation with combined ω-3 and ω-6 EFAs have ranged in duration from three to six months and include both single-site and multi-center studies (Table 15) [872–877]. A 2014 meta-analysis that considered the overall efficacy of PUFA supplementation for treating DED concluded that, compared with placebo, these interventions resulted in a significant reduction in both symptom score (quantified using the OSDI) and in the rate of cells positive for HLA-DR [878]. A Cochrane systematic review protocol on this topic was also published in 2014 and is currently in progress [879].
The role of ω-3 and/or ω-6 EFA supplementation for treating DED is not yet completely understood. Although a sizeable number of clinical trials have been conducted (Tables 13–15), most have been of short duration and show contrasting findings. There are few high-quality, randomized controlled clinical trials to inform practice. As a result, there is currently a lack of consensus in relation to the optimal protocol, in particular to the dose, composition or duration of treatment. Furthermore, most clinical studies have not measured compliance to the study interventions with blood serum fatty acid assays. This is considered essential to precisely assess the health effects of supplementation, particularly as common sources of ω-3 EFAs (such as fish oil supplements) have potential gastro-intestinal side effects that include fishy after-taste and diarrhoea, which can negatively impact compliance [880]. A large-scale, multi-center, randomized, placebo-controlled trial (DREAM study) assessing the efficacy and safety of ω-3 PUFAs (dosed at 2000 mg EPA + 1000 mg DHA/day) over 24 months, funded by the National Institute of Health, is currently underway (https://clinicaltrials.gov/ct2/show/NCT02128763). This study is predicted to inform treatment recommendations for using high-dose ω-3 PUFAs for treating DED.
Lactoferrin is a multifunctional tear glycoprotein with anti-bacterial, anti-inflammatory and anti-angiogenic properties. Tear lactoferrin levels are considered an indicator of lacrimal secretory function [881]. Reduced tear lactoferrin levels have been reported in a number of clinical populations with DED [881–886], providing scientific rationale to evaluate the potential benefit of dietary supplementation with lactoferrin as a dry eye intervention. Oral lactoferrin preserves lacrimal gland function in aged mice by reducing oxidative damage and suppressing gland inflammation [887]. In a pilot study of seven individuals with Sjögren syndrome, oral lactoferrin supplementation (270 mg/day) for one month, improved dry eye symptoms, TBUT, ocular surface vital staining scores, corneal sensitivity and impression cytology scores, with reversal of improvement upon treatment cessation [888]. A recent single-center, prospective, randomized, controlled clinical trial reported improvement in dry eye symptoms, TBUT and Schirmer scores, relative to placebo, with daily oral lactoferrin post-operatively for two months (350 mg/day) following small incision cataract surgery [889]. Further research is necessary to clarify the role of lactoferrin supplementation for treating DED.
Oxidative stress, which generates cell-damaging reactive oxygen species, may be involved in the cellular injury that leads to OSD, including dry eye [890]. In a crossover, placebo-controlled, randomized trial involving an orally-administered antioxidant supplement (containing beta-carotene, vitamins E, C, B, B6, D, zinc and copper) in individuals with marginal DED, relative improvements in tear stability, goblet cell density and squamous metaplasia were demonstrated at the one-month study endpoint [891]. Another small randomized, controlled clinical trial of a combination antioxidant and mineral (zinc) oral supplement reported improvements in TBUT and Schirmer scores, as well as reduced ocular symptoms in people with DED, compared with placebo over 12 weeks [892]. An open-label, non-controlled pilot trial involving 13 subjects with DED showed that daily oral antioxidant supplementation, with Aristotelia chilensis berry extract (30 mg), resulted in relative improvements in dry eye symptoms and Schirmer scores, compared with baseline, over two months [893].
Alpha-lipoic acid, a naturally occurring disulfide compound, also has anti-oxidant capacity [894]. In an animal model of post-menopausal dry eye, dietary supplementation with alpha-lipoic acid for 16 weeks was found to increase the activity of lacrimal peroxidase and improve lacrimal production [895]. Whether alpha-lipoic has clinical application in DED in humans remains to be investigated.
Kawashima and colleagues showed that calorie restriction preserves lacrimal gland function by attenuating oxidative damage in the lacrimal gland, suggesting that dietary changes and a reduction in calorific intake may prove beneficial in the management of dry eye [896]. More recent work from the same group in both a rat dry eye model and human clinical trial has shown the short-term value of dietary changes on dry eye signs and symptoms [897]. A recent cross-sectional single-visit study also supported the notion that increased body fat may result in an increase in dry eye symptoms [898]. Alcohol intake induces transient dry eye in healthy individuals [899], suggesting that its consumption may aggravate symptoms and signs of dry eye.
Recently, the use of spectacles containing extracts of four medicinal plants with reported antioxidant and anti-inflammatory properties, three times daily for eight weeks, was described to improve both subjective and objective signs of dry eye, compared with a placebo intervention, in individuals with mild DED [900]. Findings from these preliminary investigations require confirmation in sufficiently large, appropriately controlled, multi-center clinical trials.
Several “environmental” factors have been implicated in DED, including systemic and topical medications, desiccating conditions, digital device use and contact lens wear [102]. Consideration of these risk factors is important because this information can provide additional information on a patient's individual response to prescribed therapy.
Modification to any relevant environmental issues are potentially useful early management options, as any initial ocular surface changes culminating in DED may be prevented or potentially reversed by removing the associated environmental risk factors.
A number of studies have shown that preservatives may be associated with allergic, toxic or inflammatory reactions, particularly in patients using topical medications on a long-term basis. Preservatives such as BAK irritate the ocular surface [98], and both symptoms (such as burning, dryness and foreign body sensation) and signs are significantly more frequent in patients using preserved glaucoma medications [901,902]. Several studies have suggested that glaucoma medications may contribute to OSD and the development of dry eye [903,904], and the severity of OSD has been correlated with the number of preserved medications in use and with glaucoma disease severity [905–907].
Two large multicenter European clinical trials showed that changing to preservative-free (PF) glaucoma medications resulted in patients experiencing significantly fewer signs and symptoms of OSD [901,902]. The PF medications available for glaucoma therapy include prostaglandin analogues (PGAs), tafluprost PF, beta-blockers, timolol maleate PF and a fixed dose combination in the form of dorzolamide/timolol PF. Preservative-free timolol has been available for several years in the USA and Europe and has fewer negative effects on OSD symptoms, signs and tear function tests [908]. Ciancaglini et al. undertook confocal microscopy of the conjunctiva and performed impression cytology to demonstrate that the use of unpreserved levobunolol was associated with fewer conjunctival changes [909]. Renieri et al. reported a crossover clinical trial of 2298 subjects switching from various BAK-preserved therapies to preservative-free dorzolamide/timolol and found improved local tolerability in 80% of the patients [910]. Uusitalo et al. switched 158 patients from BAK-preserved latanoprost to preservative-free tafluprost for 3 months [911]. They found significant decreases in symptoms, corneal fluorescein staining, conjunctival hyperemia, abnormal conjunctival cells (based on HLA-DR and MUC5AC) and improvements in TBUT and Schirmer scores.
In addition to the availability of PF drugs, alternative preservatives have been developed to minimize the toxic effect of BAK [912]. Polyquaternium-1 (Polyquad®) is a quaternary ammonium preservative considered less toxic to the ocular surface, based on studies examining toxicity to corneal and conjunctival epithelial cells. Labbe et al. [913] showed that Polyquad induced considerably less toxicity than BAK in vivo and produced similar results to the control for the Schirmer test, slit-lamp, corneal fluorescein staining and histology [913]. SofZia™ is an oxidative preservation system used in one preparation of travoprost and several studies have shown improvement in symptoms and signs of OSD after switching from BAK-preserved medications to sofZia-preserved drops [914–916].
Further information on preservative interactions with the ocular surface can be found in the TFOS DEWS II Iatrogenic Dry Eye Report [102].
Many drugs used for treating chronic illnesses can contribute to DED. A higher incidence of dry eye has been reported in individuals using antihistamines, beta-blockers, antidepressants, diuretics, anxiolytics, antipsychotics, anti-Parkinsonian drugs, isotretinoin, estrogen therapy and systemic chemotherapy [102,917]. The strategies to reduce or eliminate systemic drug-induced side effects include changing the route of administration from oral to topical, discontinuation of the drugs, dose adjustments, switching to another medication or more aggressive management of the induced dry eye [102].
Blinking is critical to maintain preocular tear film homeostasis on the ocular surface [918]. Decreased blink rate or incomplete blinking affect tear dynamics, lengthening the period during which the ocular surface is exposed to water loss before the next blink, thus contributing to the development of DED [919,920]. A major factor that impacts blink rate is the use of video display terminals (VDTs) and other digital devices, reading and a variety of other visual tasks and cognitive functions. With the exponential increase of computer use in the workplace, a proportionate increase in the number of reports on the epidemiology and pathology of this condition has been reported [921,922]. The percentage of office workers using VDTs and diagnosed with dry eye increased up to 10% in male and 20% in female Japanese office workers [923]. The main mechanisms by which VDTs may induce dry eye signs or symptoms include increased tear film evaporation rate, development of MGD at an earlier age, reduced tear volume [924,925], decreased MUC5AC concentration in the tears [926] and increase oxidative stress [927].
The main treatment for individuals exhibiting such ocular surface changes is prevention of desiccation, and frequent use of ocular lubricants without preservatives is often the initial treatment of choice. However, devices or computer software that stimulate blinking on a more frequent basis represent a potential mechanism for minimizing the effect of VDTs. Miura et al. showed that a novel light-emitting diode (LED) device increased blink frequency for both dry eye and control groups [928]. Cardona et al. presented a strategy in which reflex blinking was elicited by a sudden distortion of the screen text to increase the spontaneous blink rate [929]. Frequent breaks and blinking awareness training are recommended for VDT users requiring prolonged periods of visual demand. Ergonomic factors such as lowering the screen allows the digital device user to gaze downward, thus exposing less ocular surface area to ambient air, reducing tear film loss and reducing symptoms of dry eye [930].
The ocular surface is the most environmentally exposed mucosal surface of the body, encountering challenges such as wind exposure, low relative humidity, temperature extremes, UV radiation, irritants, pollutants and tobacco smoke. Exposure to adverse ambient conditions such as low humidity and/or increased/decreased air temperature and/or air movement, leads to increased tear instability and evaporation [931]. These conditions promote the development of dry eye symptoms in normal individuals and also worsen symptoms and signs in those with DED [932–935]. Chronic dryness of the ocular surface results in a downstream cascade of events that promote inflammation, epithelial apoptosis, loss of goblet cells and changes in the meibomian glands. Studies have demonstrated the efficacy of certain treatments in response to unfavorable environmental conditions. These include the use of artificial tears [43,936,937], medications that suppress inflammatory responses [584,842,938–940], drugs that induce mucus secretion [941], and drugs that decrease apoptosis [942].
While avoiding exposure to adverse conditions that can increase tear instability and evaporation is the initial tactic, creating conditions that mimic an adequate environment for the ocular surface is also a valid approach. These include the use of humidifiers [317,943] and retention of tear fluid using moisture chamber spectacles, contact lenses and punctal plugs [307,944–946].
Increased air pollution is associated with dry eye [947] and factors such as cigarette smoking may result in a dysfunctional tear film [948–950]. Tobacco smoke contains many oxidizing and toxic substances, exposing inhalers to an enormous free radical load. Matsumoto et al. confirmed the deleterious effect of chronic cumulative tobacco smoke exposure on the tear film, resulting in an increase in tear hexanoyl-lysine levels, an oxidative stress marker for lipid peroxidation [951]. Similar findings were observed by Rummenie et al. following passive cigarette smoke exposure [952]. The adverse effects of passive tobacco smoke on the tear film is evidenced by an increase in tear inflammatory cytokines, lipid peroxidation products and a decrease in mucosal defense, resulting in instability and damage to the ocular surface epithelia [948,951]. Inhibition of the oxidative stress therapeutically might act to “break the cycle” of cytotoxicity, inflammation and cell death.
There are many factors that contribute to contact lens related discomfort and DED, including issues relating to the contact lens (including lens material, design, fit, replacement period and lens care system) [953], and the ocular surface [954]. A previous TFOS report addressed strategies to reduce contact lens discomfort [500]. These strategies included adjusting the contact lens replacement frequency, eliminating or changing the care system, altering lens design, adding tear supplementation and punctal occlusion [500].
In conclusion, there are many environmental factors that clinicians need to consider when treating individuals with DED and suitable management strategies will often be a helpful supplement to any prescribed therapies.
Due to various economic, cultural and regulatory issues, many countries exhibit a shortage of approved drugs for DED. A range of complementary medicines have been used as alternative strategies for the management of DED.
Topical and oral herbal and natural products have been widely used in many countries for thousands of years. However, relatively few RCTs have compared herbal medicine with conventional therapies due to the inherent challenges in the way herbs are prescribed. Many of these therapies are based on the traditional “yin” and “yang” theory of Chinese medicine, and therefore require that practitioners treat dry eye patients with a combination of different Chinese herbs [955]. While this potentially allows for treatments to be “tailored” to the individual, it also prevents them from being standardized, and therefore it is more difficult to study the efficacy of these products using the gold standard RCT approach. Some laboratory-based Level 1 studies have suggested that Chinese medicines may play a role in regulating the immune balance of Th1 to Th2 cells in serum, as well as the expression of aquaporin-1 and aquaporin-5 [956,957]. However, the mechanism of action of such products remains elusive and clear demonstration of the effectiveness of herbs in treating DED requires further work. There are also a number of reported side effects, including nausea, abdominal pain, diarrhoea, minor gastrointestinal symptoms, mild hepatic dysfunction and renal dysfunction that need to be considered when adopting such treatment options [958].
In a Level 1 study involving 80 participants, Chi-Ju-Di-Huang-Wan, a commonly prescribed herb, was shown to significantly improve the TBUT of dry eye subjects after 4 weeks [959]. Several Level 2 and 3 studies have investigated the optimal combination of herbs needed to treat Sjögren syndrome [444,955,958]. A Level 1 double-masked RCT with 240 subjects showed that a six-week course of ShengJinRun ZaoYangXue granules for primary Sjögren syndrome improved the symptoms of dry mouth, dry eye, and low tear flow rates, although there was no improvement in clinical signs [960].
For centuries, some cultures have considered that bee products, such as royal jelly and honey, exhibit medicinal properties. In a variety of lab-based and clinical Level 2 and 3 studies these products have been reported to have antibacterial, anti-inflammatory, antioxidant and wound healing properties [961–964]. Oral administration of royal jelly can restore tear secretion capacity in a blink-suppressed rat dry eye model [965]. Topical application of M?nuka honey eye drops can reduce the number of bacteria isolated from the eyelid margin and conjunctiva in patients with DED [966]. A M?nuka honey Cyclopower microemulsion eye cream with antimicrobial activity confirmed in preclinical testing [967], has demonstrated safety in a Phase I human tolerability trial [968]. Although promising, further clinical trials are needed to assess the therapeutic role of this formulation and other bee products.
Breast milk is a relatively common traditional medicine for treating a variety of eye conditions in some countries [969,970]. Topical instillation of breast milk, especially colostrum, has been shown to be effective in treating infant epiphora in a Level 3 study [971], and preventing neonatal conjunctivitis in a Level 1 study [972], through inhibition of a variety of common ocular pathogens [973–975].
In a small Level 3 study, 10 of 11 patients reported improvement in dryness symptoms and demonstrated some improvement in clinical signs after being treated with bovine colostrum lactoserum [976]. A rabbit study showed that topical fucosyl-lactose, a natural oligosaccharide in human colostrum, can significantly improve tear volume and TBUT in an atropine-induced dry eye model [977]. Breast milk also contains abundant lactoferrin (see section 6.3), which makes it a potent candidate for a natural remedy for dry eye treatment.
Acupuncture is a long-standing intervention in East Asian countries to treat a wide variety of conditions. However, there are no common methods for acupuncture, which makes it challenging to study in a systematic manner. It has been suggested that stimulation of the peripheral nervous system with a concomitant central effect could be the mechanism of pain relief, which might then impact pain perception, alter inflammation or peripheral sensations, or “retrain” peripheral nerves in pain sensation [978].
Acupuncture has been reported to improve TBUT, Schirmer scores and corneal staining to a greater degree than artificial tears in Level 1 studies [979,980], a Level 2 study [981], and a meta-analysis report [982]. Another Level 1 study demonstrated that tear volume, as assessed by changes in tear meniscus parameters, was significantly improved after a four week treatment with acupuncture [983]. Some studies have assessed the effects of related procedures in the management of DED. Two well-controlled clinical studies showed that both laser acupuncture and silver spike point (SSP) electro-therapy were as effective as traditional acupuncture in alleviating symptoms and increasing tear secretion in subjects with dry eye [984,985].
One shortcoming of many of these studies is that the control used to assess the relative efficacy of acupuncture was artificial tears, as opposed to sham needling. In one RCT, 42 participants with DED were enrolled to accept either “true” or sham acupuncture [986]. After four weeks, subjects from both groups reported a significant improvement in symptoms, with no significant differences between the two groups. This led the authors to conclude that sham and true acupuncture were equally effective for treating symptoms of DED.
The management of DED is complicated due to its multifactorial etiology. Expanding upon the simple credo that “diagnosis precedes therapy” means that clinicians must make their best efforts to identify the degree to which EDE (likely related to MGD), ADDE and/or other ocular surface conditions are contributing to the patient's presentation. This aspect of determining the major causative factors behind the DED is critical to appropriate management.
Fig. 1 presents, diagrammatically, an approach to the management of DED. Prior to selecting the appropriate management to undertake, questioning and diagnostic testing must be undertaken to determine that the patient does indeed have DED and then whether they are broadly showing more signs of EDE or ADDE. Further details on the appropriate tests to confirm a diagnosis of DED and then the major etiological factors can be found in the TFOS DEWS II Diagnostic Methodology Report [10]. Following confirmation of a DED diagnosis, disease severity along with etiological subtyping, will allow an appropriate treatment plan to be developed.
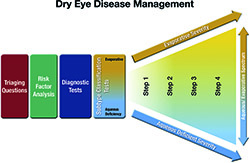
The majority of patients with DED show some relationship between symptom severity and signs. However, it is well established that a proportion of patients exhibit conflicting signs and symptoms [996–998]. In situations where there are chronic symptoms but limited signs that are refractory to treatment, then neuropathic pain, rather than DED, should be considered. This is described in greater detail in the TFOS DEWS II Pain and Sensation Report [539]. In contrast, in patients where there are few symptoms but clear signs of DED, then reduced corneal sensitivity, suggestive of neurotrophic keratopathy, is a possibility [999–1001], and prescribing treatment may be particularly important to avoid ongoing damage.
The ultimate aim of DED management is to restore homeostasis of the ocular surface, by breaking the vicious cycle of the disease, and offering long-term options to prevent a return to the vicious cycle and a resurgence of symptoms. While there are treatments that may be specifically indicated for one particular aspect of an individual patient's ocular surface condition, a number of treatments might appropriately be recommended for multiple aspects of a DED presentation. The management of DED typically involves dealing with chronic sequelae that require ongoing management, rather than short-term treatment, to eliminate the dry eye issues.
The management algorithm presented in this report does not represent a rigid stepwise approach, but rather should be viewed as an organizational tool to use when initiating treatment of DED, to select interventions likely to provide most benefit. The algorithm takes into account both disease etiology and severity, progressing from more generalized treatments for disease of mixed etiology, to more advanced and specific treatments aimed at particular aspects of the disease pathophysiology. Risk/benefit and cost considerations will also necessarily contribute to choices made between treatment options [5–9,17].
Management algorithms are often constructed to recommend a sequence of treatments according to the stage of disease, but this not possible for DED as it is a complex condition that varies, both in severity and in character, from patient to patient. Nonetheless, with the intention of assisting eye care practitioners to fashion a logical, evidence-based treatment approach, the following management algorithm (Table 16) is proposed. For patients who do not respond to a given level of management, or who exhibit more severe DED, the next level of management is recommended and, in some cases, the previous therapy may be continued, in addition to any new therapies (Fig. 1 and Table 16). In general, management approaches begin with conventional, low-risk and commonly available therapies such as over-the-counter lubricants for early stage disease, and progress to more advanced therapies for more severe forms of DED [1002]. However, it is acknowledged that the significant heterogeneity that exists in the DED patient population precludes an overly formulaic approach and it would be anticipated that these recommendations would be adapted, by eye care practitioners, to best suit individual patients.
It is important, after initiating any of these management strategies, that careful follow-up occurs to ensure patients are successfully instituting the recommended management option(s) and to establish improvements in symptoms and/or signs. The time frame over which therapy should be applied before it can be concluded that no improvement will occur is related to both the individual response and the therapy being considered. A review of the literature suggests that most studies are conducted for 1–3 months (with the exception of cyclosporine, where therapeutic action can take several months to occur and study periods are typically longer than 3 months) [595–597] and so changes beyond this time period for the majority of treatments would appear unlikely.
If there is clinical evidence of more severe complications associated with the dry eye presentation, such as advanced eyelid involvement (chalazia, trichiasis), corneal neovascularization or clinical signs of microbial infection, the clinician will need to consider additional approaches. Examples could potentially include intralesional steroid or excision of chalazia, eyelash epilation or cryotherapy for trichiasis, and antiangiogenic drugs for neovascularization. A full outline of these management strategies is beyond the scope of this report.
In summary, the management of DED remains something of an art, not easily lending itself to a rigid, evidence-based algorithm that accommodates all patients with dry eye symptoms and signs. All eye care providers who treat DED must exercise their clinical expertise to judge the significance of each of the varied pathogenic processes (aqueous deficiency, MGD, inflammation, etc.) that may manifest similar subjective complaints and similar signs of disrupted ocular surface homeostasis. On-going research will continue to improve our understanding of the relative treatment efficacy of different interventions for individual causes of DED, and determine synergistic therapeutic actions.
Table 1
Research evidence grading scheme.
Clinical Studies |
|
|
Level 1 |
Evidence obtained from at least one properly conducted, well-designed, randomized, controlled trial, or evidence from well-designed studies applying rigorous statistical approaches |
|
Level 2 |
Evidence obtained from one of the following: a well-designed controlled trial without randomization, a well-designed cohort or case-control analytic study, preferably from one or more center, or a well-designed study accessible to more rigorous statistical analysis |
|
Level 3 |
Evidence obtained from one of the following: descriptive studies, case reports, reports of expert committees, expert opinion |
|
Basic Science Studies |
|
|
Level 1 |
Well-performed studies confirming a hypothesis with adequate controls published in a high-impact journal |
|
Level 2 |
Preliminary or limited published study |
|
Level 3 |
Meeting abstracts or unpublished presentations |
Table 2
Comparative studies investigating lubricating eye drops and liposomal sprays for the management of dry eye disease.
Author, Year |
N |
Study period |
Treatment groups |
Parameters with significant improvements |
Parameters without significant effect |
|
Korb et al., 2005 [141] |
40 |
15 min |
Soothea, Systane |
LLT improved with both drops. (Soothea 107%; Systane 16%) |
None |
|
Scaffidi & Korb, 2007 [142] |
41 |
15 min |
Refresh Dry Eye Therapy drops; Soothea drops |
LLT improved with both drops; Soothea > increase than Refresh Dry Eye Therapy |
NA |
|
Wang et al., 2007 [177] |
67 |
4 weeks |
Carbomer-based, cellulose-based, and mineral oil-based artificial tear formulations |
Total scores, symptoms, signs, and Schirmer all improved. Symptoms improved with Carbomer-based formulation. |
None |
|
Craig et al., 2010 [178] |
22 |
30, 60, 90, 135 min |
Tears Again (Optrex ActiMist) liposomal spray |
LLT, tear film stability, NIBUT, comfort. |
TMH |
|
Wang et al., 2010 [179] |
30 |
4 weeks |
Carbomer-based lipid-containing gel (CBLC), HP-guar gel |
Schirmer and patient subjective assessment were both improved. CBLC > HP-guar. |
None |
|
Pult et al., 2012 [180] |
80 |
10 min |
Optrex ActiMist (AM), DryEyesMist (DEM), |
OSDI, NIBUT were both improved by AM |
DEM & TM decreased comfort and NIBUT |
|
Tomlinson et al., 2013 [65] |
37 |
2 weeks |
Carmellose sodium, carmellose sodium with lipid, glycerine with lipid drops |
Evaporation, TBUT, osmolarity, symptoms. |
None |
|
Mutalib et al., 2015 [181] |
9 (rabbits) |
2 weeks |
Virgin coconut oil, Tears Naturale II, |
None |
NIBUT |
|
Simmons et al., 2015 [182] |
256 |
3 months |
1 marketed lipid drop, |
Symptoms, OSDI, |
Corneal staining, conjunctival staining, meibomian glands, Schirmer |
LLT – lipid layer thickness, N - number of subjects; NIBUT – non-invasive break up time; OSDI – ocular surface disease index; TBUT – tear break up time.
a The Soothe formulation used in these studies is marketed today as Soothe XP.
Table 3
Clinical studies investigating the use of autologous serum for the management of dry eye disease.
Author |
Evidence level |
N |
Indication |
Follow-up |
% Serum and diluent |
Controls |
Improved |
No improvement |
|
Noble et al., 2004 [213] |
RCT (Level 1) |
16 |
SS & KCS |
3 M |
50% (0.9 NaCl) |
Crossover: Lubricants |
Symptoms, GCD |
|
|
Kojima et al., 2005 [214] |
RCT (Level 1) |
10 |
SS & non-SS according to Jap DEG |
2 W |
20% (0.9% NaCl) |
AT upre |
Symptoms, TBUT, CFS |
Schirmer score |
|
Noda-Tsuruya et al., 2006 [215] |
RCT (Level 1) |
12 |
LASIK |
6 M |
20% (0.9% NaCl) |
AT |
TBUT, CFS |
Symptoms, Schirmer score |
|
Yoon et al., 2007 [216] |
RCT (Level 1) |
41 |
SS, non-SS |
2 M |
20% (0.9 NaCl) |
Umbilical cord serum |
Symptoms, TBUT, CFS, GCD; Better symptoms, CFS (at 2 M) |
Schirmer score, corneal sensitivity, tear clearance |
|
Urzua et al., 2012 [217] |
RCT (Level 1) |
12 |
Severe non-SS based on DEWS criteria |
2 W (cross over after 7 day washout) |
20% AS |
AT |
Symptoms (OSDI) |
Fluorescein staining, TBUT |
|
Celebi et al., 2014 [218] |
Double-masked RCT (Level 1) |
20 |
Schirmer < 5 mm, TBUT <5s, OSDI >40, CFS ≥1 |
1 M |
20% (0.9% NaCl) |
Cross-over, Refresh upre |
Symptoms, TBUT |
Schirmer score, CFS |
|
Hussain et al., 2014 [219] |
Retrospective chart review |
63 |
Any patient using AS between June 2008 and January 2013 for at least 3 months |
Up to 48 M |
50% (0.9% NaCl) |
None |
Schirmer score, OSDI, CFS |
|
|
Hwang et al., 2014 [186] |
Cohort comparison (Level 2) |
20 |
1° SS* |
1 M |
50% |
2° SS* |
1° SS*: Symptoms, CFS, TBUT |
2° SS*, possibly due to increased pro-inflammatory cytokine levels |
|
Jirsova et al., 2014 [220] |
Interventional (Level 2) |
17 |
Schirmer I < 5mm/5min; TBUT < 5 s; severe symptoms as defined in DEWS |
3 M |
20% |
None |
Schirmer score, various symptoms, CFS, Impression cytology |
TBUT, TMH, dryness, discomfort |
|
Lopez-Garcia et al., 2014 [221] |
RCT (Level 1) |
26 |
SS |
2 M |
20% (0.9 NaCl) |
AS 20% diluted with HA in contralateral eye |
Symptoms, TBUT, CFS, GCD improved in both, but better in HA-AS |
Schirmer score, VA |
|
Semeraro et al., 2014 [184] |
Cohort comparison (Level 2) |
26 |
Acute OSD (Dry eye, neurotrophic keratitis, Recurrent erosion) |
16-31 W |
50% (0.9% NaCl) |
Chronic OSD |
Epithelial defects all healed |
18% recurrence in chronic OSD after cessation of AS |
|
Aggarwal et al., 2015 [222] |
Interventional (Level 2) |
16 |
Photoallodynia (excluded those with OSD) |
3 M |
20% AS |
None |
Subbasal corneal nerve density & morphology, symptoms of photophobia |
GCD density |
|
Li et al., 2015 [223] |
RCT (Level 1) |
18 |
SSSchirmer <5 mm, TBUT <5s, CFS >5 |
6 W |
50% (0.9 BSS) |
Silicone hydrogel contact lens |
Symptoms, TBUT, CFS, but symptoms and CFS better in control |
Schirmer score, BCVA |
|
Mukhopadhyay et al., 2015 [224] |
RCT (Level 1) |
52 |
Schirmer < 5 mm |
18 W - 6 on and 12 off treatment) |
20% (0.9% NaCl) |
(1) AT (2) cord blood serum |
Symptoms, TBUT, CFS |
Schirmer score |
1°/2° - primary/secondary (*historical classification); 2 M − 2 months; AS – autologous serum; AT - Artificial tears; CFS - corneal fluorescein staining; CL - contact lens; GCD - Goblet cell density; GVHD - Graft versus host disease; HA – Hyaluronic acid; KCS – keratoconjunctiovitis sicca; Jap DEG - Japanese Dry Eye Group; LASIK – laser in-situ keratomileusis; M − Months; N - number of subjects treated with serum; NaCl – saline; OSD - Ocular surface disease; OSDI – ocular surface disease index; Oxford - punctate epitheliopathy score; RCT - Randomized controlled trial; s – seconds; SS – Sjögren syndrome; TBUT – tear breakup time; upre – unpreserved; VA – visual acuity; W – Weeks.
Table 4
Level 2 studies of punctal occlusion in dry eye disease.
Author |
Subject group |
N |
Treatment duration (months) |
Reported benefits |
Comments |
|
Balaram et al., 2001 [283] |
Dry eye with plug |
50 |
6 |
Improved symptoms |
37% plug loss; more likely to lose plugs inserted in upper puncta |
|
Kojima et al., 2002 [308] |
Dry eye with silicone plug |
51 |
21 |
Improved symptoms, epithelial damage |
55.9% plug loss |
|
Nava-Castaneda et al., 2003 [309] |
Dry eye with collagen and silicone plug |
61 |
2 |
Improved symptoms, vital staining |
|
|
Farrell et al., 2003 [310] |
Dry eye with collagen plug |
62 |
0.3 |
Improved symptoms, tear function |
Benefit of occluding only lower puncta |
|
Altan-Yaycioglu et al., 2005 [311] |
Dry eye with collagen and silicone plug |
24 |
|
Improved tear function |
Similar results with both types |
|
Miyata et al., 2006 [272] |
Dry eye with atelocollagen plug |
28 |
2 |
Improved tear function, vital staining, TBUT, Schirmer score |
|
|
Chen et al., 2007 [312] |
Dry eye with Smart plug |
54 |
13 |
Improved symptoms, vital staining |
|
|
Hirai et al., 2012 [270] |
Dry eye with atelocollagen plug |
37 |
2 |
Improved symptoms, ocular surface status |
|
|
Yung et al., 2012 [257] |
Dry eye post-LASIK with plug |
18 |
3 |
Improved symptoms, tear function |
|
|
Kaido et al., 2012 [252] |
Short TBUT patients with plug |
43 |
1 |
Improved symptoms, tear function, vital staining |
|
|
Shi et al., 2013 [313] |
Dry eye with silicone plug |
65 |
6 |
Improved symptoms, corneal staining, TBUT and Schirmer score |
|
|
Capita et al., 2015 [274] |
Dry eye SS with hypromellose occlusion |
38 |
2 |
Improved symptoms, corneal staining and Schirmer score |
|
|
Tong et al., 2016 [263] |
Moderate dry eye with punctal plug |
29 |
0.75 |
Improved symptoms, corneal staining |
No changes in tear cytokines |
LASIK - laser in-situ keratomileusis; N - number of subjects; SS – Sjögren syndrome; TBUT – tear break up time.
Table 5
Level 2 studies of lid hygiene in dry eye disease.
Author |
Subject group |
N |
Lid hygiene variations |
Treatment duration (months) |
Reported benefits |
|
Paugh et al., 1990 [394] |
MGD |
21 |
Lid scrub + massage |
0.5 |
Improved TBUT |
|
Key et al., 1996 [386] |
Chronic blepharitis (80% wore CL) |
25 |
Lid scrub vs hypo-allergenic bar soap |
4 |
Improved symptoms and lid appearance |
|
Romero et al., 2004 [387] |
MGD |
37 |
Lid hygiene + heated saline + AT |
1.5 |
Improved symptoms and TBUT |
|
Guillon et al., 2012 [395] |
Blepharitis and MGD |
40 |
Lid hygiene with wipes (Blephaclean) |
3 |
Improved eyelid margin status |
|
Guillon et al., 2012 [396] |
Blepharitis and MGD |
40 |
Lid hygiene with wipes (Blephaclean) |
3 |
Improved symptoms |
|
Doan et al., 2012 [397] |
Chronic blepharitis |
33 |
Lid hygiene with cleansing solution (Blephagel) |
0.75 |
No changes in TBUT and VA; routine was well tolerated |
|
Khaireddin et al., 2013 [398] |
Chronic blepharitis and contact lens wear |
53 |
Lid hygiene (baby shampoo) |
1 |
Improved symptoms |
|
Arrua et al., 2015 [399] |
Chronic blepharitis |
45 |
Lid hygiene neutral shampoo |
2 |
Improved symptoms and signs |
|
Ngo et al., 2017 [400] |
DED |
20 |
Combination of AT, lid cleanser (TheraTears SteriLid) and oral omega-3 supplements (TheraTears Nutrition) |
3 |
Improved symptoms and signs |
AT – artificial tears; CL – contact lens; MGD – meibomian gland dysfunction; N - number of subjects; TBUT – tear breakup time; VA – visual acuity.
Table 6
Level 2 studies related to management of Demodex and dry eye disease.
Author |
Subject group |
N |
Treatment variations |
Treatment duration (months) |
Reported benefits |
|
Kheirkhah et al., 2007 [409] |
Chronic blepharitis with ocular Demodex |
6 |
TTO 50% weekly lid scrub + daily TT shampoo |
2 |
Reduced Demodex count, improved ocular irritation and inflammatory corneal signs |
|
Gao et al., 2007 [410] |
Ocular Demodex |
11 |
TTO 50% weekly lid scrub + daily TT shampoo |
1 |
Reduced Demodex count |
|
Holzchuh et al., 2011 [411] |
Refractory blepharitis with ocular Demodex |
12 |
Oral ivermectin |
1 |
Reduced Demodex count, improved tear functions |
|
Filho et al., 2011 [412] |
Chronic blepharitis with ocular Demodex |
19 |
Oral ivermectin |
3 |
Reduced Demodex count |
|
Koo et al., 2012 [413] |
Ocular Demodex |
106 |
TTO daily lid scrub |
1 |
Reduced Demodex count, improved ocular comfort |
|
Gao et al., 2012 [414] |
Ocular Demodex |
24 |
TTO 5% ointment massage |
1 |
Reduced Demodex count, improved ocular itching |
|
Salem et al., 2013 [415] |
Ocular/skin Demodex |
30 |
Oral ivermectin vs ivermectin + metronidazole |
1 |
Reduced Demodex count |
N - number of subjects; TT – tea tree; TTO – tea tree oil.
Table 7
Studies of lipid-containing eye drops in dry eye disease.
Author |
Evidence Level |
Patient group |
N |
Treatment duration |
Reported benefits |
Comments |
|
Korb et al., 2005 [141] |
2 |
Mild to severe DED |
40 |
Single drop of each type |
Increased LLT emulsion > aqueous drop |
Test 1 = oil-in-water emulsion, Test 2 = aqueous eye drop |
|
Scaffidi et al., 2007 [142] |
2 |
Mild to severe DED |
41 |
Single drop of each type |
Increased LLT |
Test 1 and 2 = two oil-in-water emulsions |
|
Maissa et al., 2010 [157] |
3 |
10 DED, 5 normals |
15 |
Single drop |
Improved symptoms, castor oil detected up to 4 h post eye drop instillation |
Test = oil-in-water emulsion |
|
McCann et al., 2012 [422] |
1 |
Mild to moderate EDE |
75 |
90 days |
Improved symptoms, evaporation, |
Test 1 = aqueous drop with sodium hyaluronate, Test 2 = aqueous drop with HMPC, Test 3 = oil-in-water emulsion |
|
Tomlinson et al., 2013 [65] |
1 |
Mild to moderate DED, age and sex-matched controls |
38 |
2 weeks |
Improved OSDI, evaporimetry, TBUT, osmolarity |
Test 1 = aqueous eye drop, |
|
Sindt et al., 2013 [423] |
2 |
Mild to moderate MGD |
49 |
4 weeks |
Improved symptoms, corneal staining, TBUT, meibomian expression |
Test = oil-in-water emulsion |
|
Aguilar et al., 2014 [424] |
1 |
Mild to moderate EDE |
49 |
4 weeks |
Improved TBUT, corneal staining, conjunctival staining, meibomian expression |
Test = oil-in-water emulsion, control = sodium chloride |
|
Kaercher et al., 2014 [425] |
3 |
Mild to severe ADDE, EDE and mixed DED |
1209 |
4 weeks |
Improved symptoms, OSDI, |
Test = oil-in-water emulsion |
|
Guthrie et al., 2015 [426] |
1 |
Symptomatic contact lens wearers |
106 |
1 month |
Improved comfort, wearing time, lid wiper epitheliopathy, corneal staining emulsion > control drops |
Test = oil-in-water emulsion, control = non-lipid containing contact lens drops |
|
Simmons et al., 2015 [182] |
1 |
Mild to moderate DED (2 with SS) |
288 |
3 months |
Improved subjective dryness symptoms, OSDI, TBUT |
Test 1, 2, 3 = three oil-in-water emulsions |
|
Ousler et al., 2015 [427] |
2 |
Moderate to severe DED |
42 |
2 weeks |
Improved symptoms, corneal staining, conjunctival staining, conjunctival redness |
Test = oil-in-water emulsion |
ADDE - aqueous deficient dry eye; DED - dry eye disease; EDE - evaporative dry eye; HPMC - hydroxypropyl methylcellulose; LLT - lipid layer thickness; MGD – meibomian gland dysfunction; N - number of subjects; OSDI – Ocular Surface Disease Index; SS – Sjögren syndrome; TBUT - tear breakup time.
Table 8
Level 1 and 2 studies of topical corticosteroids for managing dry eye disease.
Author |
Subject group/Drug |
N |
Treatment duration |
Reported benefits |
Comments |
|
Marsh & Pflugfelder, 1999 [547] |
SS. Non-preserved 1% methylprednisolone |
21 |
2 weeks |
Improved symptoms, corneal staining, filamentary keratitis |
Retrospective case series. Prolonged treatment for up to 6 months resulted in increased IOP and cataracts |
|
Sainz de la Maza Serra et al., 2000 [548] |
SS. Non-preserved 1% methylprednisolone |
15 |
2 months |
Improved symptoms, corneal staining |
Prospective. 15 subjects treated with punctal plugs post corticosteroid. Further 15 subjects also treated with punctal plugs alone. |
|
Avunduk et al., 2003 [549] |
KCS with or without SS. 3 groups: ATS only; ATS plus NSAID (flurbiprofen); ATS plus topical corticosteroid (0.1% FML) |
32 |
1 month |
ATS plus corticosteroid group had improved symptoms, reduced CFS and rose bengal staining, improved goblet cell appearance and reduced inflammatory cells |
Prospective, Single-masked, RCT |
|
Pflugfelder et al., 2004 [550] |
KCS. 0.5% loteprednol etabonate vs vehicle |
64 |
1 month |
Improved symptoms and hyperemia in more severe subjects |
Prospective, double-masked, placebo-controlled, RCT. No increase in IOP over placebo |
|
Lee et al., 2006 [551] |
KCS. 0.1% prednisolone drops in one eye and 0.1% HA drops in the other |
41 |
1 month |
Improved symptoms, NGF levels and impression cytology scores in prednisolone-treated eyes only |
Prospective, double-masked, RCT |
|
Yang et al., 2006 [552] |
KCS. 0.1% FML |
30 |
1 month |
Improved symptoms, CFS, Schirmer score, tear breakup time, conjunctival hyperemia |
Prospective, non-masked |
|
Jonisch et al., 2010 [553] |
OSD. 0.01% dexamethasone (unpreserved) |
31 |
3 months |
65% reported moderate or complete resolution of symptoms, 22% had mild improvement and 13% had no change in symptoms. No relevant elevation in IOP. |
Retrospective chart review |
|
Sheppard et al., 2014 [554] |
Mild to moderate DED. Loteprednol etabonate (LE) or ATS before the initiation of topical cyclosporine A (CsA) therapy |
61 |
6 weeks |
LE pre-treatment significantly reduced CsA stinging. Both groups showed significantly improved OSDI scores, with LE showing more OSDI improvement. Both pre-treatment strategies improved symptoms, Schirmer scores, CFS, lissamine staining, and adjunctive ATS use. |
Prospective, multicenter randomized double-masked parallel group |
|
Kheirkhah et al., 2015 [555] |
KCS due to MGD. 3 groups: ATS only; loteprednol etabonate 0.5%; loteprednol etabonate 0.5% + tobramycin 0.3% |
60 |
1 month |
Subjects treated with ATS or loteprednol alone with near-normal baseline subbasal nerve fiber demonstrated significant improvement in symptoms and CFS |
Prospective, double-masked, RCT |
|
Lin & Gong, 2015 [556] |
SS. 0.1% FML and 0.1% HA vs 0.5% CsA and 0.1% HA |
40 |
2 months |
Improved symptoms, CFS, conjunctival hyperemia, GCD, TBUT (FML > CsA) |
Prospective, parallel-group, RCT |
|
Pinto-Fraga et al., 2016 [557] |
KCS. 0.1% FML vs PVA ATS |
41 |
21 days |
Subjects treated with FML maintained the status of their ocular surface after exposure to the adverse environment; those treated with PVA tears had notable impairment in corneal and conjunctival staining and hyperaemia |
Prospective, double-masked, placebo-controlled, RCT. Included 2 h adverse environment exposure |
ATS – artificial tear solution; CFS – corneal fluorescein staining; CsA – cyclosporine A; FML – fluorometholone; GCD – goblet cell density; HA – hyaluronic acid; IOP – intraocular pressure; KCS – keratoconjunctivitis sicca; MGD – meibomian gland dysfunction; N - number of subjects; NGF – nerve growth factor; NSAID - nonsteroidal anti-inflammatory drops; OSD – ocular surface disease; OSDI – ocular surface disease index; PVA – polyvinyl alcohol; SS - Sjögren's syndrome; TBUT – tear break up time.
Table 9
Level 1 and Level 2 studies of topical cyclosporine for the management of dry eye disease.
Author |
Subject group |
N |
Treatment duration (months) |
Reported benefits |
Comments |
|
Level 1 studies |
|||||
|
Baiza-Duran et al., 2010 [588] |
Moderate to severe DED (Hispanics) |
183 |
3.5 |
Improved dryness, tearing, FBS, TBUT, corneal staining, Schirmer score |
Aqueous solution 0.1% and 0.05% |
|
Chen et al., 2010 [589] |
Moderate to severe DED (Chinese) |
233 |
2 |
Improved dryness, FBS, corneal staining, Schirmer score |
Emulsion formulation with BAK |
|
Su et al., |
Mild to severe DED |
100 |
6 |
Improved OSDI, TBUT, corneal staining, conjunctival staining, Schirmer score |
Once daily vs. twice daily dosage |
|
Deveci et al., 2014 [591] |
SS |
26 |
1 |
Improved pain, burning, TBUT, Schirmer score |
|
|
Level 2 studies |
|||||
|
Salib et al., 2006 [592] |
Post LASIK DED |
42 |
3 |
Improved Schirmer score |
|
|
Perry et al., 2008 [593] |
Mild, moderate and severe DED |
158 |
3 |
Improved OSDI, TBUT, Schirmer score, corneal staining, conjunctival staining |
|
BAK – benzalkonium chloride; DED – dry eye disease; FBS – foreign body sensation; LASIK – laser in-situ keratomileusis; N - number of subjects; OSDI - ocular surface disease index; SS - Sjögren syndrome; TBUT - tear break up time.
Table 10
Published meta-analyses of topical cyclosporine for the management of dry eye disease.
Author |
# reviewed/total # pts |
Symptom benefit |
Signs benefit |
Comments |
|
Alves et al., 2013 [594] |
6 studies/1514 |
In all studies |
In all studies |
|
|
Sacchetti et al., 2014 [595] |
18 studies/2479 |
Improved symptoms in 100% of studies, |
Improved Schirmer score in 72%, corneal staining in 53%, TBUT in 47% |
Great heterogeneity in grading scales, duration of treatment |
|
Zhou et al., 2014 [596] |
12 studies/1660 |
Improved OSDI |
Improved Schirmer score with anesthesia, TBUT |
|
|
Wan et al., 2015 [597] |
12 studies/1367 |
|
Improved OSDI, TBUT, corneal staining, Schirmer score without anesthesia, GCD |
|
DED - dry eye disease; GCD – goblet cell density; TBUT - tear break up time; OSDI - Ocular Surface Disease Index.
Table 11
Level 1 studies of topical cyclosporine treatment for the management of evaporative dry eye/meibomian gland dysfunction.
Author |
N |
Treatment duration (months) |
Symptom benefit |
Signs benefit |
|
Perry et al., 2006 [599] |
33 |
3 |
|
Lid inflammation, MG inclusions |
|
Rubin et al., 2006 [600] |
30 |
3 |
Visual blur, burning, itching |
Schirmer score, TBUT, secretion quality |
|
Schechter et al., 2009 [601] |
37 |
3 |
OSDI |
TBUT, Schirmer score, corneal staining |
|
Prabhasawat et al., 2013 [602] |
70 |
3 |
OSDI |
TBUT, lid inflammation, MG expressibility |
MG – meibomian gland; N - number of subjects; OSDI - ocular surface disease index; TBUT – tear break up time.
Table 12
Level 1, 2 and 3 studies of azithromycin for managing dry eye disease.
Author |
Subject group |
N |
Treatment variations |
Treatment duration (months) |
Reported benefits |
|
Luchs et al., 2008 [730] |
Blepharitis |
21 |
Topical 1% |
0.5 |
Improved symptoms and signs |
|
Haque et al., 2010 [731] |
Severe blepharitis |
26 |
Topical 1% |
1 |
Improved symptoms and signs |
|
Igami et al., 2011 [720] |
Severe blepharitis |
13 |
Oral 500 mg/day for 3 days in 3 cycles with 7-day intervals |
1.8 |
Improved symptoms and signs, tear function |
|
Optiz et al., 2011 [732] |
Blepharitis |
33 |
Topical 1% |
1 |
Improved symptoms and signs |
|
Nichols et al., 2012 [733] |
Contact lens dry eye |
50 |
Topical 1% |
1 |
Improved symptoms and signs |
|
Fadlallah et al., 2012 [734] |
Severe blepharitis |
67 |
Topical 1.5% |
3 |
Improved symptoms and signs |
|
Hosseini et al., 2016 [735] |
Blepharitis |
907 |
Topical 0.1% dexamethasone; topical 1% azithromycin; combination of both; vehicle |
0.5 |
Improved symptoms and signs in the combination and 0.1% dexamethasone groups |
Table 13
Major published intervention clinical trials of oral ω-3 EFA supplementation for dry eye disease.
Author, Year |
N |
Study period |
Oral ω-3 intervention (daily dose) |
Control |
Evidence level |
Parameters with significant improvements relative to controlg |
Parameters without significant effect relative to controlg |
|
Macsai, 2008 [849]. |
38f |
12 months |
Flaxseed oil 3300 mg |
Placebo (olive oil) |
1 |
Primary: Symptoms (OSDI) |
Secondary: TBUT, meibum scores, Schirmer score, corneal staining. |
|
Wojtowicz et al., 2011 [850] |
36 |
90 days |
EPA 450 mg + DHA 300 mg + flaxseed oil 100 mg |
Placebo (wheatgerm oil) |
1e |
Symptoms (OSDI) |
Schirmer score, evaporimetry, lipid composition of MG secretions, TBUT |
|
Bhargava et al., 2013 [851] |
518 |
3 months |
EPA 650 mg + DHA 350 mg |
Placebo (corn oil) |
1 |
Symptoms, TBUT and Schirmer score |
Rose bengal staining and conjunctival impression cytology |
|
Olenik et al., 2013 [852] |
61b |
3 months |
EPA 127.5 mg + DHA 1050 mgc |
Placeboc (sunflower oil) |
1 |
Symptoms (OSDI), TBUT, lid margin inflammation, MG expression and Schirmer score |
None |
|
Kawakita et al., 2013 [853] |
27 |
12 weeks |
EPA 1245 mg + DHA 540 mg |
Placebo (middle chain triglycerides) |
1 |
Symptoms and TBUT |
Schirmer score, ocular surface fluorescein or rose bengal staining |
|
Kangari et al., 2013 [854] |
64 |
30 days |
EPA 360 mg + DHA 240 mg |
Placebo (middle chain triglycerides) |
1 |
Primary: TBUT |
None |
|
Pinazo-Duran et al., 2013 [855] |
66d |
3 months |
EPA 85 mg + DHA 700 mg + 60 mg DPA + antioxidant |
None (open-label) |
2 |
Not applicable |
Reduced inflammatory tear cytokines (relative to baseline only) |
|
Olenik, 2014 [856] |
905 |
12 weeks |
EPA 127.5 mg + DHA 1050 mg + DPA 90 mg |
None (open-label) |
2 |
Not applicable |
Symptomsa (relative to baseline only) |
|
Bhargava, 2015 [857] |
256 |
45 days |
EPA 720 mg + DHA 480 mg |
Placebo (olive oil) |
1 |
Primary: Symptoms. |
Secondary: Schirmer score |
|
Deinema et al., 2017 [858] |
60 |
90 days |
Krill oil (EPA 945 mg + DHA 510 mg) and Fish oil (EPA 1000 mg + DHA 500 mg) |
Placebo (olive oil) |
1 |
Primary: Tear osmolarity and symptoms (OSDI). Secondary: TBUT, Ocular bulbar redness, tear levels of the pro-inflammatory cytokine IL-17A. |
Secondary: NIBUT, Schirmer score, TMH, levels of other tear cytokines IL-2, IL-4, IL-6, IL-10, IFN-gamma, TNF-alpha. |
|
Epitropoulos et al., 2016 [859] |
105 |
12 weeks |
EPA 1680 mg + DHA 560 mg re-esterified ω-3 EFAs |
Safflower oil (3136 mg) |
1 |
Primary: Tear osmolarity. Secondary: TBUT, Symptoms (OSDI), MMP-9 positivity. |
Secondary: Corneal fluorescein staining, Schrimer test. |
DHA - docosahexaenoic acid; DPA - docosapentaenoic acid; EPA - eicosapentaenoic acid; IFN – interferon; IL – interleukin; MG - meibomian gland; MMP-9 – matrix metalloproteinase-9; N - number of subjects; NIBUT – non-invasive tear break up time; OSDI - ocular surface disease index; TBUT - tear break up time; TMH, tear meniscus height; TNF – tumor necrosis factor.
a No objective clinical measurements were evaluated.
b Study population involved only individuals with MGD.
c Both the intervention and control groups were instructed to also undertake eyelid hygiene and use non-preserved artificial tears, each day, throughout the study.
d Study population involved both individuals with DED (n = 30) and healthy controls (n = 36).
e Double-masked, randomized controlled pilot study, which was inadequately powered to detect significant differences between the study groups.
f Study population involved individuals with MGD and blepharitis.
g Primary and secondary outcomes are specified when defined by the authors.
Table 14
Major published interventional clinical trials of oral ω-6 EFA supplementation for dry eye disease.
Author, Year |
N |
Study period |
Oral ω-6 intervention (daily dose) |
Control |
Evidence level |
Parameters with significant improvements relative to controlf |
Parameters without significant effect relative to controlf |
|
Manthorpe et al., 1984 [867] |
36c |
3 weeks |
cis-linoleic acid 365 mg + GLA 45 mg |
Placebo |
1 |
Schirmer test score |
TBUT, lissamine green staining, tear lysozyme and corneal sensitivity |
|
Oxholm et al., 1986 [868] |
28c |
8 weeks |
cis-linoleic acid 2190 mg + GLA 270 mg |
Placebo |
1 |
None |
No improvements in Schirmer score, TBUT or lissamine green staining |
|
Theander et al., 2002 [869] |
90c |
6 months |
Two doses tested: |
Placebo (corn oil) |
1 |
None. |
No improvements with either dose for eye pain, dry eye symptoms, Schirmer test or lissamine green staining |
|
Barabino et al., 2003 [872] |
26d |
45 days |
LA 57 mg + GLA 30 mge |
Placeboe |
1 |
Symptoms, reduced conjunctival HLA-DR expression and lissamine green staining. |
TBUT, Schirmer test score |
|
Aragona et al., 2005 [870] |
40c |
1 month |
LA 112 mg + GLA 15 mg |
Placebo (fructose) |
1 |
Symptoms, increased levels of tear PGE1 and CFS |
TBUT, tear basal secretion |
|
Pinna et al., 2007 [871] |
57a |
6 months |
LA 28.5 mg + GLA 15 mg |
None |
2b |
Not applicable |
Symptoms, MG secretion turbidity and MG obstruction (relative to baseline only) |
CFS – corneal fluorescein staining; GLA - gamma-linolenic acid; HLA-DR - human leukocyte antigen D-related; LA - linolenic acid; N - number of subjects; PGE1-prostaglandin E1; TBUT - tear break up time.
a Study population involved only individuals with MGD.
b Investigator-masked only.
c Study population involved only individuals with primary Sjögren syndrome.
d Study population involved only individuals with aqueous-deficient DED.
e Both the intervention and control groups were instructed to use non-preserved artificial tears, each day, throughout the study.
f Primary and secondary outcomes are specified when defined by the authors.
Table 15
Major published intervention clinical trials of combined oral ω-3 and ω-6 EFA supplementation for dry eye disease.
Author, Year |
N |
Study period |
Oral ω-6 intervention (daily dose) |
Control |
Evidence level |
Parameters with significant improvements relative to controla |
Parameters without significant effect relative to controla |
|
Creuzot et al., 2006 [873] |
71 |
6 months |
EPA 28 mg + DHA 392 mg + GLA 82 mg + LA 126 mg |
Placebo (basic oleic acid) |
1b |
Reflex tearing and bulbar hyperemia |
Schirmer score, TBUT, ocular surface fluorescein and lissamine green staining |
|
Larmo et al., 2010 [874] |
86c |
3 months |
Sea buckthorn oil (2 g): long chain ω-3 EFAs 149 mg + ω-6 245 mg |
Placebo (medium-chain triglycerides) |
1 |
Bulbar redness and ocular burning |
Tear osmolarity, Schirmer score, TBUT |
|
Brignole-Baudouin et al., 2011 [875] |
106 |
3 months |
EPA 427.5 mg + DHA 285 mg + borage oil 15 mg + zinc 10 mg + vitamins |
Placebo (medium-chain triglycerides) |
1 |
Reduction in percentage of conjunctival HLA-DR positive cells. |
Schirmer score, TBUT and ocular surface staining |
|
Jackson et al., 2011 [876] |
43 |
6 months |
ALA 1000 mg + GLA 500 mg |
ALA 1000 mg + GLA 500 mg + topical cyclosporine 2× daily for the last 3 months |
2d |
Not applicable |
Both groups showed improvements in symptoms and TBUT relative to baseline only |
|
Creuzot-Garcher et al., 2011 [877] |
181 |
6 months |
EPA 28 mg + DHA 392 mg + GLA 82 mg + LA 126 mg |
Placebo (basic oleic acid) |
1 |
TBUT, reduced ocular fatigue score |
Schirmer score, ocular surface staining. |
|
Sheppard et al., 2013 [878] |
38e |
6 months |
ALA 196 mg + EPA 128 mg + DHA 99 mg + DPA 39 mg + LA 710 mg + GLA 240 mg |
Placebo (sunflower oil) |
1 |
Symptoms (OSDI), corneal surface asymmetry index and conjunctival HLA-DR expression |
TBUT, conjunctival fluorescein and lissamine green staining, Schirmer score. |
ALA - alpha-linolenic acid; DHA - docosahexaenoic acid; DPA - docosapentaenoic acid; EFAs – essential fatty acids; EPA - eicosapentaenoic acid; GLA - gamma-linolenic acid; HLA-DR - human leukocyte antigen D-related; LA - linolenic acid; OSDI – ocular surface disease index; N - number of subjects; TBUT - tear break up time.
a Primary and secondary outcomes are specified when defined by the authors.
b Masking procedures are unclear.
c Both intervention and control groups included contact lens wearers.
d Neither clinical outcome assessors or participants were masked (open-label study).
e Study population involved only post-menopausal women.
Table 16
Staged management & treatment recommendations for dry eye diseasea,b,c.
Step 1:
|
|
|
|
Step 2:
|
|
|
|
Step 3:
|
|
|
|
Step 4:
|
MGD – meibomian gland dysfunction; DED – dry eye disease.
a Potential variations within the disease spectrum are acknowledged to exist between patients and the management options listed above are not intended to be exclusive. The severity and etiology of the DED state will dictate the range and number of management options selected from one or more steps.
b One or more options concurrently within each category can be considered within that step of the dry eye disease state. Options within a category are not ranked according to importance and may be equally valid.
c It should be noted that the evidence available to support the various management options differs and will inevitably be lower for newer management options. Thus, each treatment option should be considered in accordance with the level of evidence available at the time management is instigated.
d The use of prescription drugs needs to be considered in the context of the individual patient presentation, and the relative level of evidence supporting their use for that specific indication, as this group of agents differs widely in mechanism of action.